| Child Kidney Dis > Volume 24(2); 2020 > Article |
|
Abstract
Nephrogenic syndrome of inappropriate antidiuresis (NSIAD) is a rare X-linked genetic condition caused by a gain-of-function mutation of arginine vasopressin receptor 2 gene, AVPR2. We report the case of a male neonate diagnosed with NSIAD based on his DNA sequence of the AVPR2 gene and the clinical course. He demonstrated a complete correction of hyponatremia using oral urea. We suggest that (1) sequencing analysis of the AVPR2 gene ought to be done in newborns with prolonged euvolemic hyponatremia, hypo-osmolality, high urinary sodium and normal/low or undetectable AVP levels, and that (2) oral urea is a safe and effective treatment option in infants diagnosed with NSIAD until the patients are grown-up.
Nephrogenic syndrome of inappropriate antidiuresis (NSIAD) is a rare X-linked genetic condition caused by a gain-of-function mutation of the vasopressin receptor 2 (V2R) gene, AVPR2 . V2R is a G-protein-coupled receptor that is located at the basolateral membrane of principal cells in the collecting duct. Upon activation by the ligand, V2R stimulates adenylyl cyclase and, thus, the production of cyclic adenosine monophosphate (cAMP). Then, cAMP activates endocytic vesicle protein kinase A (PKA). Endocytic vesicle PKA phosphorylates aquaporins and finally, phosphorylated aquaporins are inserted into the principal cell membrane to transmit water through the epithelial layer [1].
The syndrome of inappropriate antidiuresis hormone secretion (SIADH) is caused by the excessive production of a V2R binding ligand [arginine vasopressin (AVP)], known as an antidiuretic hormone. SIADH is one of the most common causes of hyponatremia in hospitalized neonates [2]. NSIAD has similar clinical manifestations to SIADH, including euvolemic hyponatremia, abnormally-increased urine osmolality and urine sodium concentration, and decreased serum osmolality. However, the serum AVP level is either undetectable or very low in patients with NSIAD [3]. Here, we report a case of AVPR2-related NSIAD in a 9-day-old male baby.
A 9-day-old male baby presented with a persistently reduced serum sodium concentration (126 mmol/L). The patient was born at 36 weeks of gestation via an elective cesarean section with a birth weight of 3,450 g (95th percentile). He did not have any perinatal complications. He had no siblings and no family history of hyponatremia. His mother was Vietnamese and treated for chronic hepatitis B. He did not show any accompanying anomalies on physical examination, except for a mild hydrocele. His blood pressure was normal. Although he had no perinatal complications, he was admitted to the neonatal intensive care unit at the age of 6 days, because of his deficient oral intake for the first 5 days of his life (150ŌĆō200 mL/day). Owing to the patientŌĆÖs oropharyngeal dysphagia, confirmed by videofluoroscopic swallowing study, we started orogastric tubefed formula (8.7 mmol/L of sodium) and breast milk. His initial laboratory workup on the day of admission revealed hyperbilirubinemia (15.0 mg/dL), hyponatremia, and low serum osmolality with normal serum levels of potassium, bicarbonate, blood urea nitrogen, creatinine, glucose, and albumin. Spot urine osmolality (mOsm/kg) and sodium concentration (mmol/L) were 117 and 28, respectively. Table 1 presents the laboratory values of the patient.
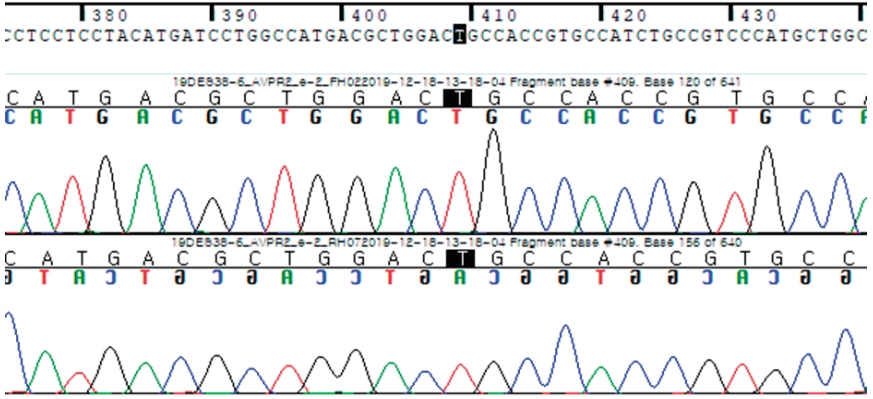
To correct serum sodium level in the patient, we administered normal saline and several hypertonic sodium chloride supplements either intravenously or orally. Since the initiation of orogastric tube feeding, the patient attained normal body weight without any gastrointestinal symptom. Although his serum sodium level remained low, the serum total bilirubin level decreased after taking milk supplements. In addition, tandem-mass inborn error of metabolism evaluation, thyroid function, and 17 alpha-hydroxyprogesterone were within reference ranges. Besides, abdominal ultrasonography and brain magnetic resonance imaging were normal. Moreover, plasma renin activity and aldosterone level were normal. Notably, the plasma AVP level was within the lower part of the reference range. Furthermore, when we performed an adrenocorticotropic hormone stimulation test; the random basal cortisol level was below the reference range and the cortisol level at 60 min after administering the synthetic corticotropin was marginally below the reference range. Thus, we started hydrocortisone (10 mg/m2/day). However, his plasma ACTH level at 8 a.m. was in normal range (46 pg/mL). Hydrocortisone was soon discontinued because the serum sodium level remained below the reference range. Table 2 presents further laboratory findings of the patient. All results were consistent with SIADH, although the plasma antidiuretic hormone level was within normal range. Thus, we sent the patient's blood to Green Cross Genome Laboratory Celemics (Yongin, Korea). The patientŌĆÖs DNA was isolated from whole blood using G-Mendeliome Diagnostics Exome Sequencing test panel of Green Cross Genome Laboratory Celemics and sequenced by NextSeq (Illumina) paired-end read method. A hemizygotic mutation was identified. Then it was confirmed and sequenced by SangerŌĆÖs method. The mutation was as follows: nucleotide 770 of the AVPR2 gene was mutated from cytosine to thymine, changing arginine to cysteine at codon 137 (R137C), as shown in Fig. 1.
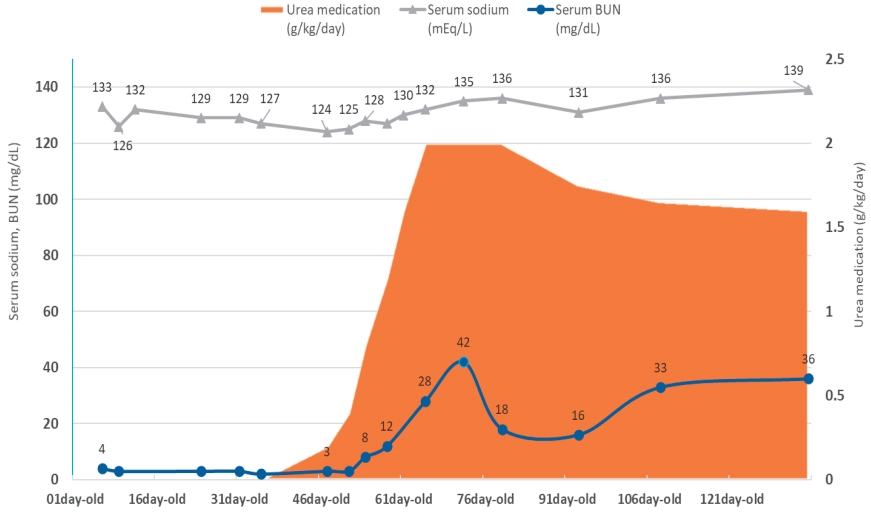
The patient was treated with oral urea per HuangŌĆÖs protocol [4]: 30% oral urea solution was started at 0.1 g/kg/day divided into four doses and increased gradually to 2 g/kg/day. For the oral urea treatment, we obtained a lime-flavored Urea solute (UreNaTM) containing 15 g of urea in one sachet. Then, the serum sodium level was normalized, and his weight gain was maintained in the reference range (Fig. 2). He is now 7 months old, being clinically well with normal growth and development. He did not show any kind of seizures due to hyponatremia. We continued to supply oral urea (2 g/kg/day) and monitor his serum sodium and BUN concentration, development and growth. Since his serum concentration of BUN is higher than the reference range, we kept the same amount of oral urea unless his serum sodium concentration is below normal range. Doing so, the dosage of oral urea is naturally decreased as he gains weight.
The volume status of the body is regulated by the thirst mechanism and urinary excretion of water. SIADH is a syndrome of excessive water reabsorption in the urinary system due to the excessive level of plasma AVP usually when there is a lesion in either the central nervous system or the lung [5].
Furthermore, hyponatremia is a common laboratory finding in hospitalized neonates. As the probability of a pathological entity is increased when the degree of hyponatremia is more severe [6], the pediatrician is usually aware of the range of the patientŌĆÖs serum sodium level, especially when the neonate patient has signs like weight loss, poor sucking power, or vomiting. Given that the volume states of neonatal period can be deteriorated easily by many factors, it is not easy to make the right diagnosis in hyponatremic neonates.
Feldman et al. described two pediatric patients with NSIAD in 2005 for the first time [3]. The patients met the diagnostic criteria for SIADH, though AVP was undetectable. Furthermore, they found mutations of the AVPR2 gene which caused a gain-of-function of V2R. Our findings are compatible to those of previously-reported cases except that he had no severe symptom like seizures or irritability.
To the best of our knowledge, this is the first case of NSIAD in South Korea, which is confirmed by a molecular biologic study. Owing to the challenges involved in determining the patientŌĆÖs volume state, our patient was initially treated for dehydration and steroid deficiency, but his hyponatremia was not treated. As the patient was treated with an oral urea solution, he demonstrated a rapid correction of hyponatremia. Also, his dysphagia with aspiration improved with oropharyngeal rehabilitation therapy, and his weight gain and development were normal. Thus, our patient was effectively treated using an oral urea solution, eventually normalizing prolonged hyponatremia.
Despite the fact that there are no guidelines for the treatment of patients with NSIAD, a few options are available. Conventional therapy applicable to mild to moderate cases involves fluid restriction. However, limiting the entry of fluids for patients in the neonatal and infantile periods is challenging, since they only consume low-salt liquid meals such as breast milk or formula. In such cases, the oral intake of urea is another option, which has been established as a cost-effective and safe treatment option for adults with chronic SIADH. Several other options have been explored in many fields to treat patients with SIADH and some scholars have also attempted to treat pediatric patients with NSIAD [4,7,8]. Our patient was also treated using an oral urea solution and we confirmed its efficacy. In some studies, tolvaptan, an antagonist of V2R, and furosemide were also used similarly. However, no results have been reported to confirm their efficacy [9,10].
Urea is a substance with a molar mass of 60 g/mol. Absorbed urea in gastro-intestinal tract distributes in total body water and it works as an effective osmole in nephron. Thus, when the patient takes urea orally, an osmotic diuresis occurs by urea and the free water excretion of the patient increases. Its distaste is well-known factor to trigger side effects like nausea or vomiting. However, there have been no reports of osmotic demyelination syndrome by oral urea treatments. Nevertheless, physician should be careful to increase the dosage of oral urea [11].
In conclusion, we suggest that: (1) genetic profiling of the AVPR2 gene or V2R receptor ought to be done in all newborns with prolonged euvolemic hyponatremia, hypoosmolality, high urinary sodium and normal/low or undetectable AVP levels, and that (2) oral urea is a safe and good treatment option in patients diagnosed with NSIAD until the patient grows up.
References
1. Bockenhauer D, Bichet DG. Urinary concentration: different ways to open and close the tap. Pediatr Nephrol 2014;29:1297-303.



2. Storey C, Dauger S, Deschenes G, Heneau A, Baud O, Carel JC, et al. Hyponatremia in children under 100 days old: incidence and etiologies. Eur J Pediatr 2019;178:1353-61.



3. Feldman BJ, Rosenthal SM, Vargas GA, Fenwick RG, Huang EA, Matsuda-Abedini M, et al. Nephrogenic syndrome of inappropriate antidiuresis. N Engl J Med 2005;352:1884-90.



4. Huang EA, Feldman BJ, Schwartz ID, Geller DH, Rosenthal SM, Gitelman SE. Oral urea for the treatment of chronic syndrome of inappropriate antidiuresis in children. J Pediatr 2006;148:128-31.


5. Baylis PH. The syndrome of inappropriate antidiuretic hormone secretion. Int J Biochem Cell Biol 2003;35:1495-9.


6. Corona G, Giuliani C, Parenti G, Norello D, Verbalis JG, Forti G, et al. Moderate hyponatremia is associated with increased risk of mortality: evidence from a meta-analysis. PLoS One 2013;8:e80451.



7. Dufek S, Booth C, Carroll A, Van't Hoff W, Kleta R, Bockenhauer D. Urea is successful in treating inappropriate antidiuretic hormone secretion in an infant. Acta Paediatr 2017;106:513-5.


8. Cailleaux A, Mahieu F, Heinrichs C, Adams B, Ismaili K, Brachet C. Nephrogenic syndrome of inappropriate antidiuresis: Early diagnosis avoids severe hyponatremia complications. Arch Pediatr 2017;24:630-3.


9. Erdelyi LS, Mann WA, Morris-Rosendahl DJ, Gross U, Nagel M, Varnai P, et al. Mutation in the V2 vasopressin receptor gene, AVPR2, causes nephrogenic syndrome of inappropriate diuresis. Kidney Int 2015;88:1070-8.


Fig.┬Ā1.
Sanger sequencing of the patient. AVPR2 Sanger sequencing result NM_000054.4:c. 409C>T, p.Arg137Cys.
Table┬Ā1.
PatientŌĆÖs Initial Laboratory Findings on Admission
Table┬Ā2.
Further Evaluation Results of the Patient
| Patient data | Reference range | |
|---|---|---|
| Serum and plasma studies | ||
| ŌĆāAldosterone (pg/mL) | 529.8, 329.4* | 60ŌĆō680 |
| ŌĆāPlasma renin activity (ng/mL/h) | 0.97, 2.37* | <15 |
| ŌĆāAVP (pg/mL) | 4.21, 5.31* | 1.0ŌĆō13.3 |
| ŌĆāTSH (uIU/mL) | 1.52 | 1.7ŌĆō9.1 |
| ŌĆāFree thyroxine (ng/dL) | 1.41 | 0.8ŌĆō1.8 |
| ŌĆāCortisol (mcg/dL) | ||
| ŌĆāŌĆāBaseline | 1.3 | 4ŌĆō20 |
| ŌĆāŌĆā60 min after intravenous synthetic corticotropin (15 mcg/kg) | 17.8 | >20 |
- TOOLS
-
 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link XML Download
XML Download Full text via DOI
Full text via DOI-
 Download Citation
Download Citation
- Download Citation
-
- Close
 Print
Print-
Share :



-
METRICS

-
- 0 Crossref
- 0 Scopus
- 4,339 View
- 68 Download
- ORCID iDs
-
Hyunwoo Bae

https://orcid.org/0000-0003-2196-6421Hee Sun Baek

https://orcid.org/0000-0003-0940-360XHae Min Jang

https://orcid.org/0000-0002-8231-2950Eun Joo Lee

https://orcid.org/0000-0003-1014-5783Min Hyun Cho

https://orcid.org/0000-0002-7965-7587 - Related articles
-
A Case of Infantile Nephrotic Syndrome associated with Neuroblastoma2018 October;22(2)
Two Cases of Nephrotic Syndrome Associated with Kimura Disease1999 October;3(2)