| Child Kidney Dis > Volume 22(2); 2018 > Article |
|
Abstract
Nephrotic syndrome in the first year of life, characterized by renal dysfunction and proteinuria, is associated with a heterogeneous group of disorders. These disorders are often related to genetic mutations, but the syndrome can also be caused by a variety of other diseases. We report an infant with nephrotic syndrome associated with a neuroblastoma. A 6-month-old girl was admitted with a 10% weight loss over 10 days and nephrotic-range proteinuria. She was ill-looking, and her blood pressure was higher than normal for her age. Her cystatin-C glomerular filtration rate was decreased, and levels of plasma renin, aldosterone, and catecholamines were elevated. Renal ultrasonography and abdominal computed tomography showed a retroperitoneal prevertebral mass encasing both renal arteries and the left renal vein. The mass was partially resected laparoscopically, and the pathologic diagnosis was neuroblastoma. Findings on a simultaneous renal biopsy were unremarkable. The patient was treated with chemotherapy and several anti-hypertensive drugs, including an alpha blocker. Two months later, the mass had decreased in size and the proteinuria and hypertension were gradually improving. In an infant with abnormal renin-angiotensin system activation, severe hypertension, and nephrotic-range proteinuria, neuroblastoma can be considered in the differential diagnosis.
Congenital nephrotic syndrome presents at birth or during the first 3 months of life, whereas infantile nephrotic syndrome is diagnosed during the first year [1]. Nephrotic syndrome in this age range is characterized by renal dysfunction and proteinuria, and it may be associated with a heterogeneous group of disorders. Nephrotic-range proteinuria is defined by a spot urinary protein-to-creatinine ratio higher than 0.25 g of protein per mmol of creatinine [2]. The most common condition in childhood is idiopathic nephrotic syndrome, which includes entities such as minimal-change nephrotic syndrome (MCNS) and focal segmental glomerulosclerosis (FSGS). Most patients with MCNS and 20% with FSGS achieve remission after 8 weeks of steroid treatment [2]. The most common etiologies of infantile nephrotic syndrome are mutations in genes that regulate the glomerular filtration barrier. Other causes in infants include congenital infections, fibrillary glomerulopathy, amyloidosis, light-chain deposit disease, cancer, systemic lupus erythematosus, hereditary disorders, and vascular problems [2,3]. We report an infant with nephrotic syndrome associated with neuroblastoma.
A 6-month-old girl was admitted with nephrotic-range proteinuria after a febrile illness. Over the preceding 10 days, her oral intake had decreased by half and her weight had dropped from 9 to 8.1 kg (a 10% decrease). She had been healthy at birth at a gestational age of 37 weeks and with a birth weight of 2,770 g. However, she had required neonatal intensive care unit for 10 days after birth due to a febrile illness. Prenatal ultrasonography had shown no remarkable findings, and there was no family history of renal disease. Her blood pressure on admission was high on repeated measurements (163/106 mmHg, above the 95th percentile for age). Her temperature was 36.9Ōäā, heart rate 156 beats/min, and respiratory rate 40 breaths/min. She appeared acutely ill. There was no lymphadenopathy, her breath sounds were clear, and there was no cardiac murmur, hepatosplenomegaly, or generalized edema.
On complete blood count, the leukocyte count was 14,800/mm3, hemoglobin 10.8 g/dL, and platelets 278,000/mm3. Arterial blood gas analysis reported a pH of 7.49, pCO2 38.0 mmHg, and bicarbonate 29 mEq/L. Blood urea nitrogen was 9 mg/dL, creatinine 0.2 mg/dL, and the cystatin-C glomerular filtration rate (GFR) 69 mL/min/1.73m2. The cholesterol was 390 mg/dL, total plasma protein 4.5 g/dL, and albumin 1.7 mg/dL. The aspartate aminotransferase was 36 IU/L, alanine aminotransferase 40 IU/l, total bilirubin 0.2 mg/dL, sodium 131 mmol/L, potassium 3.5 mmol/L, and chloride 94 mmol/L. The C-reactive protein was 1.06 mg/dL (normal range 0ŌĆō0.6 mg/dL) and B-type natriuretic peptide 272 pg/mL (normal range 0ŌĆō100 pg/mL). Immunoglobulin and complement levels were all within the normal ranges. The plasma renin activity was 40.0 ng/mL/h (normal range 0ŌĆō1.16 ng/mL/h), aldosterone 242 ng/dL (normal range 5ŌĆō90 ng/dL), cortisol 8.4 ug/dL (normal range 5-25 ug/dL), parathyroid hormone 22.1 pg/mL (normal range <0.90 pg/mL), epinephrine 148.8 pg/mL (normal range <50 pg/mL), norepinephrine 3,375.2 pg/mL (normal range 110ŌĆō410 pg/mL), and plasma normetanephrine 12.33 nmol/L (normal range <0.90 nmol/L), while the metanephrine level was normal at 0.46 nmol/L (normal range <0.50 nmol/L). These laboratory results are summarized in Table 1.
Urinalysis revealed a spot urine albumin-to-creatinine ratio of 19,792 mg/g and a spot urine protein-to-creatinine ratio of 19,098.4 mg/g. The pH was 7.0 and specific gravity 1.015. A urine culture was sterile.
Initial ultrasonography was unremarkable. However, because the serum renin and aldosterone were increased, we repeated the ultrasonography to search for a cause of renal hypertension. The repeat renal imaging revealed a heterogeneous, echogenic, 3.9├Ś1.9 cm mass with internal calcifications in the midline of the upper abdomen. There was swelling of the left kidney with increased parenchymal echogenicity and a poorly differentiated corticomedullary junction. Abdominal computed tomography (CT) demonstrated that the mass was located prevertebrally, surrounding the anterior margin of the abdominal aorta and encasing the celiac axis, both renal arteries, and the inferior vena cava at the insertion site of the left renal vein (Fig. 1). There was a size discrepancy of the kidneys, with the left kidney measuring 7.5 cm and the right 6.3 cm. There was decreased enhancement of the right kidney, and lymphadenopathy were noted in both the paraaortic area and portocaval space. Renal Doppler ultrasonography showed asymmetric high resistive index values in the left kidney, suggesting partial compression of the left renal vessels by the mass. On echocardiography, ventricular function appeared normal, as was the cardiac structure.
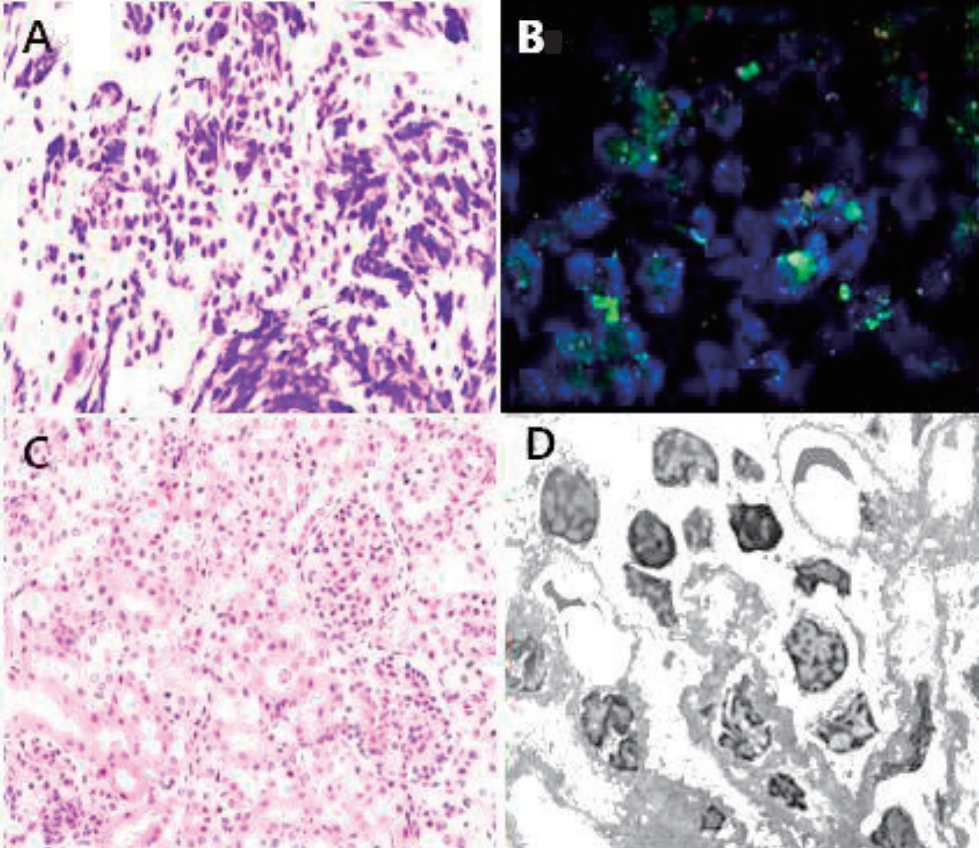
The patient underwent laparoscopic excisional biopsy of the mass and a right kidney biopsy. The frozen section of the mass revealed a neuroblastoma. The serum neuron specific enolase was elevated at 32.4 ng/mL. Histopathology of the mass showed a poorly differentiated, N-myc-negative neuroblastoma with favorable histology. Evaluation of the renal tissue specimen revealed glomeruli of normal size and distribution, with no evidence of crescent formation or sclerosis. The mesangium, interstitium, tubules, and blood vessels were all unremarkable. On transmission electron microscopy, there were no electron-dense deposits or focal effacement of foot processes (Fig. 2).
To address the nephrotic syndrome and hypertension, the patient was treated with deflazacort, 2.25 mg/kg/day, and anti-hypertensive drugs, including an alpha blocker. An angiotensin converting enzyme (ACE) inhibitor was added before chemotherapy was started. The latter consisted of 4 cycles of carboplatin, etoposide, cyclophosphamide, and doxorubicin. Her blood pressure and proteinuria gradually improved during chemotherapy, eventually reaching levels normal for her age. Most of the drugs therefore could be discontinued except for the ACE inhibitor. After chemotherapy, the spot urine protein-to-creatinine ratio decreased to 381.2 mg/g. Follow-up abdominal CT showed that the neuroblastoma had decreased in size to 1.4├Ś1.1├Ś2.4 cm over 2 months. After chemotherapy was completed, the neuroblastoma was even smaller and subsequently remained stable and she underwent excision operation of residual neuroblastoma. Serum albumin levels increased, and the serum renin activity and aldosterone level decreased to 25.1 ng/mL/h (normal range 0ŌĆō1.16 ng/mL/h) and 16.9 ng/dL (normal range 5ŌĆō90 ng/dL).
In adults, nephrotic syndrome is known in some cases to be associated with cancer and a worse cancer prognosis [4]. In a large population-based cohort in Denmark between 1980 and 2010, Christian et al. suggest nephrotic syndrome was associated with lung cancer and kidney cancer. The association between nephrotic syndrome and cancer was most marked for hematologic malignancies [4]. MCNS suggests possible HodgkinŌĆÖs disease, while membranous nephropathy is more suggestive of carcinoma [5]. Membranoproliferative and focal sclerosis renal lesions also occur with a variety of tumors. There is considerable evidence that, in cases of carcinoma and nephrotic syndrome, the renal lesion is generally due to immune complexes, involving either tumor-associated antigens, fetal antigens, or viral antigens [5].
However, the coexistence of nephrotic syndrome and a neoplasm is rarely found in children [6]. Two previous reports reveal the association of nephrotic syndrome with a neuroblastoma [7,8]. A case of neuroblastoma in a 4-year-old boy presenting with nephrotic syndrome was reported in 1979. His renal biopsy demonstrated membranous glomerulonephritis with deposition of neuroblastoma-associated immune complexes in the glomerular basement membrane [8]. Another case was about a 10-month-old child with neuroblastoma presented with acute kidney injury, a hyponatremic-hypertensive-like syndrome, and nephrotic proteinuria [7].
In the present case, because the neuroblastoma encased both renal arteries and the left renal vein, there was partial compression of the renal vessels by the tumor mass, with disruption of the renal blood supply. Compression of the renal vein is not only a common cause of treatable hypertension, but it also increases intraglomerular pressure and renin activity [9]. Increased intraglomerular pressure has been shown to induce glomerular hyperfiltration with proteinuria and activation of the renin-angiotensin system (RAS) with increase in renin activity [10,11]. The nephroticrange proteinuria and the hypertension in our patient were exacerbated by the increased renin production. RAS activation also leads to increases in angiotensin II, which in turn increases the permeability of the glomerular membrane [10,12]. This mechanism may explain the development of nephrotic syndrome in this patient with a neuroblastoma compressing the renal vessels.
As an embryonal malignancy of the sympathetic nervous system, neuroblastoma can also be associated with elevated plasma catecholamine levels, which may, along with renal artery compression, contribute to severe hypertension [13]. More than 90% of neuroblastoma excrete catecholamines (dopamine, epinephrine, norepinephrine, metanephrine, metanephrine, normetanephrine and phenolic acid). Of these catecholamine metabolites, vanillylmandelic acid and homovanillic acid are most commonly analysed in urine of neuroblastoma patients [14]. In the two previously published cases of nephrotic syndrome associated with neuroblastoma, one patient had a normal blood pressure, but the other had hypertension [7,8]. The first child had catecholamine levels in the normal range except for normetanephrine and noradrenaline [7]. The other child, a 4-year-old boy, had a blood pressure higher than normal for his age and increased urine levels of homovanillic acid [8].
On admission, our patientŌĆÖs cystatin-C GFR was below normal at 69 mL/min/1.73m2. This presumably indicated impaired renal function due to bilateral compression of the renal arteries. Renal-artery stenosis may occur in combination with renal insufficiency. In patients with renal-artery stenosis and renal failure, renal revascularization may improve or stabilize renal function [9]. In our patient, after 4 cycles of chemotherapy, a repeat cystatin-C GFR was back in the normal range at 105 mL/min/1.73m2.
As noted above, there are few reported cases of infantile nephrotic syndrome associated with a neuroblastoma. The initial presentation of neuroblastoma may vary considerably from case to case depending on where it arises in the widespread sympathetic nerve system [15]. This case illustrates that neuroblastoma may present with RAS system activation, hypertension, and nephrotic-range proteinuria. Hence, neuroblastoma can be considered in the differential diagnosis of that constellation of findings.
References
1. Jalanko H, Holmberg C. Congenital nephrotic syndrome. Pediatr Nephrol; Springer: 2009. p. 601-19.
4. Christiansen CF, Onega T, Sv├”rke C, Farkas DK, Jespersen B, Baron JA, et al. Risk and prognosis of cancer in patients with nephrotic syndrome. Am J Med 2014;127:871-7.e1.


5. Papper S. Nephrotic syndrome and neoplasm: the findings to date, with practical implications. Postgrad Med 1984;76:147-58.


6. Bacchetta J, Juillard L, Cochat P, Droz J-P. Paraneoplastic glomerular diseases and malignancies. Crit Rev Oncol Hematol 2009;70:39-58.


7. Poggi GM, Fognani G, Cuzzubbo D, Liguori A, Resti M, Pela I. Neuroblastoma presenting with acute kidney injury, hyponatremichypertensive-like syndrome and nephrotic proteinuria in a 10-month-old child. Case Rep Oncol 2011;4:400-5.



8. Zheng H-L, Maruyama T, Matsuda S, Satomura K. Neuroblastoma presenting with the nephrotic syndrome. J Pediatr Surg 1979;14:414-9.


10. Cachat F, Bogaru A, Micheli J-L, Lepori D, Guignard J-P. Severe hypertension and massive proteinuria in a newborn with renal artery stenosis. Pediatr Nephrol 2004;19:544-6.


11. Szerlip , Harold M, Bhupinder Singh. Renal Artery Stenosis: Diagnosis and Management. Cardio-Nephrology. Springer, Cham 2017;411-8.

12. Peleg H, Bursztyn M, Hiller N, Hershcovici T. Renal artery stenosis with significant proteinuria may be reversed after nephrectomy or revascularization in patients with the antiphospholipid antibody syndrome: a case series and review of the literature. Rheumatol Int 2012;32:85-90.


13. Pio L, Avanzini S, Mattioli G, Martucciello G, Sementa AR, Conte M, et al. Perioperative management of hypertensive neuroblastoma: A study from the Italian Group of Pediatric Surgical Oncologists (GICOP). J Pediatr Surg 2017;52:1633-6.


14. Verly IR, van Kuilenburg AB, Abeling NG, Goorden SM, Fiocco M, Vaz FM, et al. Catecholamines profiles at diagnosis: Increased diagnostic sensitivity and correlation with biological and clinical features in neuroblastoma patients. Eur J Cancer 2017;72:235-43.


15. Maris J, Hogarty M, Bagatell R. Neuroblastoma Lancet 369: 2106-2120, 2007 Crossref. Medline.
Fig.┬Ā1.
Abdominal computed tomography in a 6-month-old girl ; Serial abdominal computed tomography (CT) views show a neuroblastoma that gradually decreased in size with treatment. (A) and (B): Initial CT shows a lobulated, low attenuating, 3.9├Ś2.2├Ś4 cm mass in the midline of the retroperitoneum (white arrow). (C) and (D): Interval decrease and stabilization in size of the neuroblastoma after chemotherapy.

Fig.┬Ā2.
Excisional biopsy specimen of the neuroblastoma; (A) Tissue from an excisional biopsy of the retroperitoneal mass (H&E, 400), demonstrating a poorly differentiated neuroblastoma with favorable histology. (B) The tissue is negative for a change in the N-myc gene copy number on fluorescent in situ hybridization. (C) Right kidney tissue (H&E, 200) showing no obvious histologic lesion. None of the glomeruli have crescent formation or sclerosis, and the mesangium is unremarkable. (D ) Right kidney tissue electron microscopy (3,000) showng no electron-dense deposits or focal foot process effacement.
Table┬Ā1.
Details in Initial and Final Laboratory Tests
| Laboratory test (normal range) | Initial | FinalŌĆĀ |
|---|---|---|
| Spot urine protein to Cr ratio | 19,098.4 mg/g | 381.2 mg/g |
| BUN/Cr | 9 mg/dL / 0.2 mg/dL | 8 mg/dL / 0.25 mg/dL |
| Cystatin-C GFR | 69 mL/min/1.73m2 | 105 mL/min/1.73 m2 |
| Total plasma protein | 4.5 g/dL | 7.0 g/dL |
| albumin | 1.7 mg/dL | 4.0 mg/dL |
| Renin (0ŌĆō1.16 ng/mL/h) | 40.0 | 25.1 |
| Aldosterone (5ŌĆō90 ng/dL) | 242 | 16.9 |
| Epinephrine (<50 pg/mL) | 148.8 | 56.0 |
| Norepinephrine (110ŌĆō410 pg/mL) | 3,375.2 | 851.5 |
| Normetanephrine (<0.90 nmol/L) | 12.33 | 2.27 |
| Metanephrine (<0.50 nmol/L) | 0.46 | 0.14 |
| Neuroblastoma size | 3.9├Ś 2.2├Ś4 cm | 1.4├Ś1.1├Ś2.4 cm* |
- TOOLS
-
 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link XML Download
XML Download Full text via DOI
Full text via DOI-
 Download Citation
Download Citation
- Download Citation
-
- Close
 Print
Print-
Share :



-
METRICS

-
- 0 Crossref
- 0 Scopus
- 6,584 View
- 90 Download
- Related articles
-
A Case of Nephrotic Syndrome with Swine-origin H1N1 Influenza Virus2010 October;14(2)
Clinical Evaluation of Nephrotic Syndrome Manifesting in the First Year of Life2009 October;13(2)