2. Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2012 Revised International Chapel Hill consensus conference nomenclature of Vasculitis. Arthritis Rheum 2013;65:1-11.


3. Mills JA, Michel BA, Bloch DA, Calabrese LH, Hunder GG, Arend WP, et al. The American College of Rheumatology 1990 criteria for the classification of vasculitis. Arthritis Rheum 1990;33:1114-21.


4. Ozen S1, Pistorio A, Iusan SM, Bakkaloglu A, Herlin T, Brik R, et al. Paediatric Rheumatology International Trials Organisation (PRINTO). EULAR/PRINTO/PRES criteria for Henoch-Sch├Čnlein purpura, childhood polyarteritis nodosa, childhood Wegener granulomatosis and childhood Takayasu arteritis: Ankara 2008. Part II: Final classification criteria. Ann Rheum Dis 2010;69:798-806.


5. Jung DY, Kwon YR, Yu MH, Namgoong MK. Cinical Features and Prognosis of Henoch-Sch├Čnlein Purpura in Children and Adults: A 13-Year Retrospective Study at a Single Centre. Child Kidney Dis 2017;21:61-8.


6. Jauhola O, Ronkainen J, Koskimies O, Ala-Houhala M, Arikoski P, H├Čltt├ż T, et al. Renal manifestations of HenochŌĆÉSch├Čnlein purpura in a 6ŌĆÉmonth prospective study of 223 children. Arch Dis Child 2010;95:877-82.


7. Saulsbury FT. Henoch-Schonlein purpura in children. Report of 100 patients and review of the literature. Medicine(Baltimore) 1999;78:395-409.


8. Calvi├▒o MC, Llorca J, Garc├Ła-Porr├║a C, Fern├Īndez-Iglesias JL, Rodriguez-Ledo P, Gonz├Īlez-Gay MA. Henoch-Sch├Čnlein purpura in children from northwestern Spain: a 20-year epidemiologic and clinical study. Medicine (Baltimore) 2001;80:279-90.


9. Narchi H. Risk of long term renal impairment and duration of follow up recommended for Henoch-Sch├Čnlein purpura with normal or minimal urinary findings: a systematic review. Arch Dis Child 2005;90:16-20.
10. Wang H, Das L Hoh SF, Gao X, Book YX, Arkachaisri T. Urinalysis Monitoring In Children With Henoch-Sch├Čnlein Purpura: Is It Time To Revise? Int J Rheum Dis 2019;22:1271-7.


11. de Almeida JL, Campos LM, Paim LB, Leone C, Koch VH, Silva CA. Renal involvement in Henoch-Sch├Čnlein purpura: a multivariate analysis of initial prognostic factors. J Pediatr 2007;83:259-66.
12. Alfredo CS, Nunes NA, Len CA, Barbosa CM, Terreri MT, Hil├Īrio MO. Henoch-Sch├Čnlein purpura: recurrence and chronicity. J Pediatr 2007;83:177-80.


14. Ju T, Cummings RD. A unique molecular chaperone Cosmc required for activity of the mammalian core 1 beta 3-galactosyltransferase. Proc Natl Acad Sci USA 2002;99:16613-8.


15. He X, Zhao P, Kang S, Ding Y, Luan J, Liu Z, et al.
C1GALT1 polymorphisms are associated with Henoch-Sch├Čnlein purpura nephritis. Pediatr Nephrol 2012;27:1505-9.



19. Amoli MM, Thomson W, Hajeer AH, Calvi├▒o MC, Garcia-Porrua C, Ollier WE, et al. Interleukin 8 gene polymorphism is associated with increased risk of nephritis in cutaneous vasculitis. J Rheumatol 2002;29:2367-70.

20. Nathwani D, Laing RB, Smith CC, Edward N. Recurrent post-infective Henoch-Schonlein syndrome: a genetic influence related to HLA B35? J Infect 1992;25:205-10.


21. Amoli MM, Thomson W, Hajeer AH, Calvi├▒o MC, Garcia-Porrua C, Ollier WE, et al. HLA-B35 association with nephritis in Henoch-Sch├Čnlein purpura. J Rheumatol 2002;29:948-9.

22. Zhou TB, Ou C, Qin YH, Luo W. A meta-analysis of the association between angiotensin-converting enzyme insertion/deletion gene polymorphism and Henoch-Sch├Čnlein purpura nephritis risk in Asian children. Clin Exp Rheumatol 2012;30:315-6.

24. Ronkainen J, Koskimies O, Ala-Houhala M, Antikainen M, Merenmies J, Rajantie J, et al. Early prednisone therapy in Henoch-Sch├Čnlein purpura: a randomized, double-blind, placebo-controlled trial. J Pediatr 2006;149:241-7.


25. Huber AM, King J, McLaine P, Klassen T, Pothos M. A randomized, placebo-controlled trial of prednisone in early Henoch Sch├Čnlein purpura. BMC Med 2004;2:7-13.


26. Dudley J, Smith G, Llewelyn-Edwards A, Bayliss K, Pike K, Tizard J. Randomized, double-blind, placebo-controlled trial to determine whether steroids reduce the incidence and severity of nephropathy in Henoch-Schonlein Purpura (HSP). Arch Dis Child 2013;98:756-63.


27. Hahn D, Hodson EM, Willis NS, Craig JC. Interventions for preventing and treating kidney disease in Henoch-Schonlein Purpura (HSP). Cochrane Database Syst Rev 2015;7:Cd005128.

29. Goldstein AR, White RH, Akuse R, Chantler C. Long-term followup of childhood Henoch-Sch├Čnlein nephritis. Lancet 1992;339:280-2.


30. Ronkainen J, Nuutinen M, Koskimies O. The adult kidney 24 yearsafter childhood Henoch-Sch├Čnlein purpura: a retrospective cohort study. Lancet 2002;360:666-70.


31. Butani L, Morgenstern BZ. Long-term outcome in children after Henoch-Schonlein purpura nephritis. Clin Pediatr (Phila) 2007;46:505-11.


32. Fogazzi GB, Pasquali S, Moriggi M, Casanova S, Damilano I, Mihatsch MJ, et al. Long-term outcome of Sch├Čnlein-Henoch nephritis in the adult. Clin Nephrol 1989;31:60-6.

33. Huang X, Wu J, Wu XM, Hao YX, Zeng CH, Liu ZH, et al. Significance of histological crescent formation in patients with IgA vasculitis (Henoch-Sch├Čnlein purpura)-related nephritis: a cohort in the adult Chinese population. BMC Nephrol 2018;22:334-43.
34. Pillebout E, Thervet E, Hill G, Alberti C, Vanhille P, Nochy D. Henoch-Sch├Čnlein Purpura in adults: outcome and prognostic factors. J Am Soc Nephrol 2002;13:1271-8.


36. Hattori M, Ito K, Konomoto T, Kawaguchi H, Yoshioka T, Khono M. Plasmapheresis as the sole therapy for rapidly progressive Henoch-Scho┬©nlein purpura nephritis in children. Am J Kidney Dis 1993;33:427-33.

38. Lan HY, Nikolic-Paterson DJ, Mu W, Vannice JL, Atkins RC. Interleukin-1 receptor antagonist halts the progression of established crescentic glomerulonephritis in the rat. Kidney Int 1995;47:1303-9.


39. Khan SB, Cook HT, Bhangal G, Smith J, Tam FW, Pusey CD. Antibody blockade of TNF-alpha reduces inflammation and scarring in experimental crescentic glomerulonephritis. Kidney Int 2005;67:1812-20.


40. L├│pez-Mej├Łas R, Casta├▒eda S, Genre F, Remuzgo-Mart├Łnez S, Carmona FD, Llorca J, et al. Genetics of immunoglobulin-A vasculitis (Henoch-Sch├Čnlein purpura): an updated review. Autoimmun Rev 2018;17:301-15.


43. Pang S, Lv J, Wang S, Yang G, Ding X, Zhang J. Differential expression of long non-coding RNA and mRNA in children with Henoch-Sch├Čnlein purpura nephritis. Exp Ther Med 2019;17:621-32.

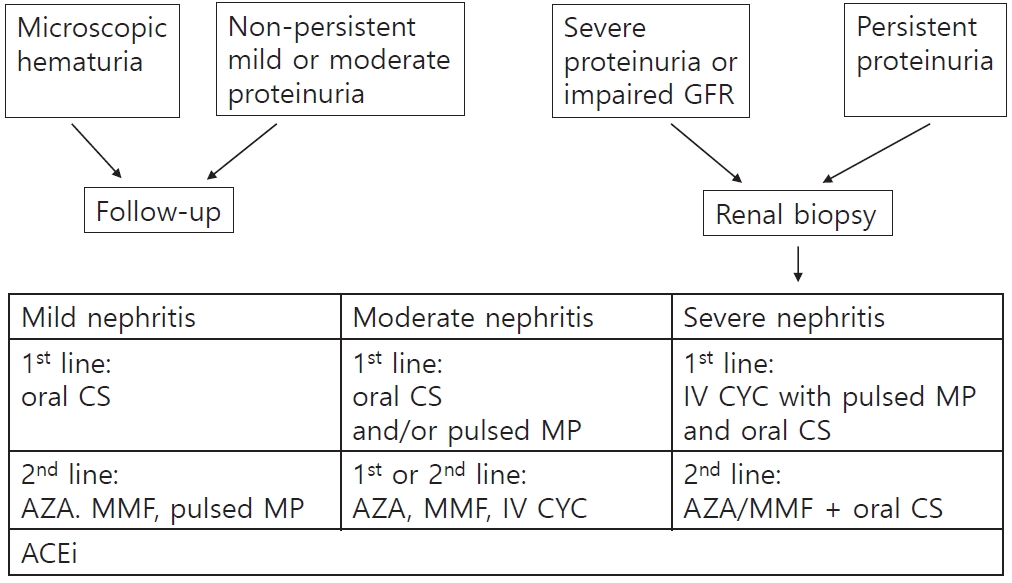
44. Kidney Disease: Improving Global Outcomes. Chapter 11: Henoch-Schonlein purpura nephritis. Kidney Int Suppl(2011) 2012;2:218-20.


45. Emancipator SN1993. . Primary and secondary forms of IgA nephritis and Sch├Čnlein-Henoch syndrome. In: Heptinstall RH. Pathology of the kidney. Little Brown; London: p. 389-476.
46. Davin JC, Ten Berge IJ, Weening JJ. What is the difference between IgA nephropathy and Henoch-Sch├Čnlein purpura nephritis? Kidney Int 2001;59:823-4.


47. Andersen RF, Rubak S, Jespersen B, Rittig S. Early high-dose immunosuppression in Henoch-Sch├Čnlein nephrotic syndrome may improve outcome. Scand J Urol Nephrol 2009;43:409-15.


51. Rauen T, Eitner F, Fitzner C, Sommerer C, Zeier M, Otte B, et al. STOP-IgAN Investigators. Intensive Supportive Care plus Immunosuppression in IgA Nephropathy. N Engl J Med 2015;373:2225-36.


53. Management and treatment of glomerular diseases (part 1): conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kid Int 2019;95:268-80.
56. Smith AC, Molyneux K, Feehally J, Barratt J. O-glycosylation of serum IgA1 antibodies against mucosal and systemic antigens in IgA nephropathy. J Am Soc Nephrol 2006;17:3520-8.


58. Block GA, Whitaker S. Maintenance of remission following completion of OMS721 treatment in patients with IgA nephropathy (IGAN). Abstract SA-PO278. J Am Soc Nephrol 2017;28:749-50.
59. Fellstr├Čm BC, Barratt J, Cook H, Coppo R, Feehally J, de Fijter JW, et al. Targeted-release budesonide versus placebo in patients with IgA nephropathy(NEFIGAN): a double-blind, randomised, placebo-controlled phase 2b trial. Lancet 2017;389:2117-27.


60. Suzuki H, Yasutake J, Makita Y, Tanbo Y, Yamasaki K, Sofue T, et al. IgA nephropathy and IgA vasculitis with nephritis have a shared feature involving galactose-deficient IgA1-oriented pathogenesis. Kidney Int 2018;93:700-5.


62. Hisano S, Matsushita M, Fujita T, Iwasaki H. Activation of the lectin complement pathway in Henoch-Schonlein purpura nephritis. Am J Kidney Dis 2005;45:295-302.


63. Abou-Ragheb HH, Williams AJ, Brown CB, Milford-Ward A. Plasma levels of the anaphylatoxins C3a and C4a in patients with IgA nephropathy/Henoch-Schonlein nephritis. Nephron 1992;62:22-6.


67. Lafayette RA, Canetta PA, Rovin BH, Appel GB, Novak J, Nath KA, et al. A Randomized, Controlled Trial of Rituximab in IgA Nephropathy with Proteinuria and Renal Dysfunction. J Am Soc Nephrol 2017;28:1306-13.


68. Tian M, Liu C. Heparin calcium treated Henoch-Schonlein purpura nephritis in children through inhibiting hyperfibrinolysis. Ren Fail 2015;37:1100-4.


69. Heeg JE, de Jong PE, van der Hem GK, de Zeeuw D. Reduction of proteinuria by angiotensin converting enzyme inhibition. Kidney Int 1987;32:78-83.


70. Remuzzi A, Perticucci E, Ruggenenti P, Mosconi L, Limonta M, Remuzzi G. Angiotensin converting enzyme inhibition improves glomerular size-selectivity in IgA nephropathy. Kidney Int 1991;39:1267-73.


72. Coppo R, Peruzzi L, Amore A, Piccoli A, Cochat P, Stone R, et al. Igace: a placeboŌĆÉcontrolled, randomized trial of angiotensinŌĆÉ converting enzyme inhibitors in children and young people with IgA nephropathy and moderate proteinuria. J Am Soc Nephrol 2007;18:1880-8.


73. Maeba S, Ichiyama T, Ueno Y, Makata H, Matsubara T, Furukawa S. Effect of montelukast on nuclear factor kappaB activation and proinflammatory molecules. Ann Allergy Asthma Immunol 2005;94:670-4.


74. Wu SH, Liao PY, Chen XQ, Yin PL, Dong L. Add-on therapy with montelukast in the treatment of Henoch-Sch├Čnlein purpura. Pediatr Int 2014;56:315-22.


75. Neufeld M, Molyneux K, Pappelbaum KI, Mayer-Hain S, von Hodenberg C, Ehrchen J, et al. Galactose deficient IgA1 (GD-IgA1) in skin and serum from patients with skin-limited and systemic IgA Vasculitis. J Am Acad Dermatol 2019;19:30443-8.


76. Vuong MT, Hahn-Zoric M, Lundberg S, Gunnarsson I, van Kooten C, Wramner L, et al. Association of soluble CD89 levels with disease progression but not susceptibility in IgA nephropathy. Kidney Int 2010;78:1281-7.


77. Papista C, Lechner S, Ben Mkaddem S, LeStang MB, Abbad L, Bex-Coudrat J, et al. Gluten exacerbates IgA nephropathy in humanized mice through gliadin-CD89 interaction. Kidney Int 2015;88:276-85.


78. Landecho MF, Ros NF, Alegre F, Idoate MA, Lucena JF. Henoch-Sch├Čnlein purpura associated with celiac disease. J Am Acad Dermatol 2011;64:e120-1.


79. Legendre P, R├®gent A, Thiebault M, Mouthon L. Anti-endothelial cell antibodies in vasculitis: a systematic review. Autoimmun Rev 2017;16:146-53.


82. Inoue CN, Matsutani S, Ishidoya M, Homma R, Chiba Y, Nagasaka T. Periodontal and ENT therapy in the treatment of pediatric henoch-sch├Čnlein purpura and IgA nephropathy. Adv Otorhinolaryngol 2011;72:53-6.

 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link XML Download
XML Download Full text via DOI
Full text via DOI Download Citation
Download Citation
 Print
Print








