| Child Kidney Dis > Volume 26(1); 2022 > Article |
|
Abstract
Purpose
Delta neutrophil index (DNI) indicates immature granulocytes in peripheral blood and has been confirmed to be effective as a prognostic factor for neonatal sepsis. Also, it has been reported to have diagnostic value in acute pyelonephritis and in predicting vesicoureteral reflux (VUR) in the infant. We conducted the study to verify whether DNI is also helpful in the entire pediatric age group with febrile urinary tract infection (UTI).
Methods
Medical records of children hospitalized for febrile UTIs were analyzed retrospectively. All subjects underwent kidney ultrasound and voiding cystourethrography. In the group with and without VUR, we compared sex and age, and the following laboratory values: the white blood cell count, neutrophil, polymorphonuclear leucocyte, eosinophil, hemoglobin, platelet count, C-reactive protein, DNI value, and the finding of ultrasound.
Results
A total of 315 patients (163 males and 152 females; range, 0ŌĆō127 months) were eligible, and 41 patients (13%) had VUR. As a result of univariate analysis, the white blood cell count, neutrophil, DNI, and ultrasonic abnormalities were high in the reflux group, and the hemoglobin and lymphocyte fraction values were low. The value of DNI and the abnormal ultrasound were significantly higher in the reflux group on the multivariate analysis. The area under the curve value of the receiver operating curve was higher in DNI (0.640; 95% confidence interval, 0.536ŌĆō0.744; P=0.004), and the DNI cutoff value for VUR prediction was 1.85%.
Urinary tract infection (UTI) is a common bacterial disease in childhood. If appropriate diagnosis and treatment are not performed early, chronic renal failure or high blood pressure may occur due to renal scars [1,2]. In particular, in infants, about 30% to 50% of children with UTIs are known to have urinary tract abnormalities [3], and vesicoureteral reflux (VUR) is common.
VUR is diagnosed in about 25% to 50% of children with febrile UTI and is well known to cause recurrent UTI and renal scar [4]. It can be diagnosed through voiding cystourethrography (VCUG), but discussions on the indication of the test have continued because it has a disadvantage in radiation exposure and invasiveness. Previously, VCUG was recommended in children between the ages of 2 months and 2 years with febrile UTI [5], but the revised the American Academy of Pediatrics (AAP) guidelines in 2011 stated that VCUG should not be performed routinely after the first febrile UTI but performed in specific circumstances [6].
Therefore, young age, high C-reactive protein (CRP) concentration, family history of urinary tract diseases, and neurosurgical abnormalities have been suggested as risk factors for VUR to predict VCUG implementation [7,8], but the association is not clearly established.
Meanwhile, immature granulocytes appear in peripheral blood in the process of promoting granulocyte production in the bone marrow during infection or systemic inflammatory reactions, and recently, these immature granules have been steadily suggested as predictors of infection or sepsis [9-11]. However, it was difficult to apply clinical trials because manual calculation is required to identify immature granules, and accuracy depends on the examiner. Delta neutrophil index (DNI) was recently proposed as a new indicator to reflect the circulating fraction of immature granules [9]. DNI is an index calculated in leukocyte identification in ADVIA 2120 (Siemens Healthineers, Erlangen Germany), one of the types of automatic blood cell analyzer [12], which has the advantage of obtaining results quickly because it is automatically calculated during complete blood cell count. Because DNI reflects the number of immature granulocytes, it has been reported to help determine the severity of patients suspected of sepsis or systemic inflammation [9,13,14], and recent studies have also reported diagnostic value in young infants with febrile UTI [15]. Lee et al. [15] identified that DNI showed a moderate specificity and low sensitivity for predicting the presence of VUR, especially in younger infants. So, the authors conducted this study to confirm the clinical usefulness of DNI as a predictor of VUR in the entire pediatric age group with febrile UTI.
From December 2002 to April 2007, the medical records of children hospitalized for febrile UTI at Konyang University Hospital in Daejeon were analyzed retrospectively. Because VCUG was selectively implemented since 2011 after the changed AAP guideline, we selected patients with febrile UTI who were treated before 2011 who underwent both kidney ultrasound (USG) and VCUG to reduce selection bias.
Among them, 315 people (163 males and 152 females) who underwent both kidney USG and VCUG were included as the study subjects. Total white blood cell count, polymorphonuclear leucocyte, total neutrophil count, CRP, hemoglobin, platelet count, DNI value, and abnormalities of USG were compared in both groups with or without VUR. Those who did not perform either test or had congenital deformities such as single kidney, bladder diverticulum, or polycystic kidney disease were excluded.
We used the blood test results performed on the hospitalization date, and the total blood cell calculation value and DNI were automatically calculated by the automatic blood cell analyzer (ADVIA 2120; Siemens Healthineers). The DNI values calculated through the ADVIA 2120 automated blood cell analyzer are as follows: DNI=(the leukocyte subfraction assayed in the myeloperoxidase channel by cytochemical reaction)ŌĆō(the leukocyte subfraction counted in the nuclear lobularity channel by the reflected light beam).
USG-positive was defined as cases whose renal USG performed by radiologist confirmed one-sided or both-sided pelviectasia or hydronephrosis, and VUR was defined as cases reflux from VCUG was confirmed.
SPSS version 25.0 (IBM Corp., Armonk, NY, USA) and R package 4.1.3 (R Foundation for Statistical Computing, Vienna, Austria) were used for statistical analysis. Through univariate and multivariate analysis and area under the curve value of the receiver operating characteristic (ROC) curve, we compared the effectiveness of the variables and obtained the cutoff value of DNI. The case of P<0.05 was judged to be statistically significant.
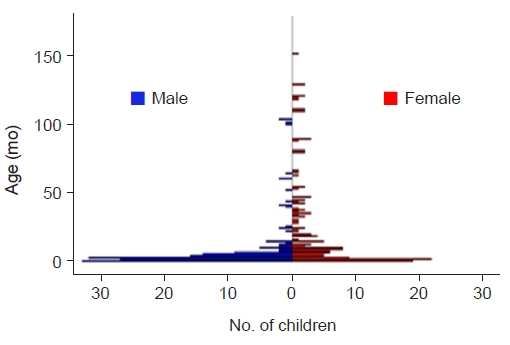
Of the 315 patients, 163 (51.7%) were boys and 152 (48.3%) were girls, and the average age was 14.0┬▒22.9 months (median, 4.7 months; range, 0ŌĆō127 months). There were 209 (66.3%) under the age of 1 year, 81 (25.7%) from 1 to 5 years of age, and 25 (7.9%) over 5 years of age, respectively (Fig. 1). There were 65 patients (20.6%) with USG-positive, and 41 patients (13.0%) diagnosed VUR on one or both sides by VCUG (Table 1).
The mean age of reflux group was 14.2┬▒20.1 months, which was not different from the group without VUR (14.0┬▒23.3 months). Girls (n=24, 58.5%) were more common in the VUR group, and boys (n=146, 53.3%) were more common in the group without VUR, but there was no statistically significant difference between the two groups. Blood tests showed no difference in eosinophil fraction (P=0.293), polymorphonuclear cell fraction (P=0.233), and platelet count (P=0.380), but the total white blood cell count (18.0┬▒6.5 ├Ś103/╬╝L vs. 15.3┬▒6.7 ├Ś103/╬╝L, P=0.013), neutrophil fraction (57.1%┬▒19.3% vs. 50.7%┬▒18.5%, P=0.039), and CRP (2.6┬▒1.6 mg/dL vs. 4.0┬▒2.0 mg/dL, P=0.003) showed higher values in the VUR group (Table 1).
The rate of abnormal findings on USG was 36.6% (15/41) in the reflux group and 18.2% (50/274) in the group without VUR (P=0.007). Even in the group with VUR, as many as 65.3% (32/49) patients showed normal findings on renal USG. In our study, the detection sensitivity of renal USG for VUR was only 34.5%. It is because VUR grades 1 and 2 do not have hydronephrosis, and grade 3 may not have hydronephrosis, depending on the status of the bladder. The DNI value was also statistically significantly higher in the reflux group (3.4%┬▒10.0% vs. ŌĆō0.2%┬▒5.6%, P=0.031) (Table 1).
As a result of multivariate logistic regression analysis, the variables that differed significantly between the group with and without VUR were CRP, kidney USG, and DNI. It means that these indices can be used to predict the existence of VUR.
The odds ratio (OR) of USG-positive, CRP, and DNI were 2.744 (95% confidence interval [CI], 1.249ŌĆō6.026; P=0.012), 1.383 (95% CI, 1.193ŌĆō1.604; P<0.001) and 1.079 (95% CI, 1.016ŌĆō1.147; P=0.014), respectively (Table 2).
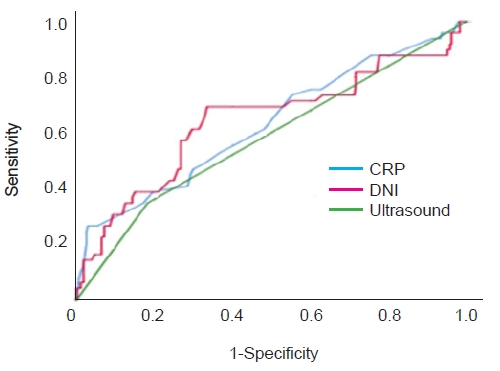
We used ROC analysis to compare the predictive capabilities of these indices. The area under the curve value of the ROC curve of the USG-positive was 0.408 (95% CI, 0.309ŌĆō0.507; P=0.058), CRP was 0.631 (95% CI, 0.540ŌĆō0.721; P=0.005), and that of DNI was 0.640 (95% CI, 0.536ŌĆō0.744; P=0.004), the highest at DNI (Table 3, Fig. 2).
UTI in children can lead to renal scars, chronic renal failure, and high blood pressure due to damage to the renal parenchyma if diagnosed early and not appropriately treated. VUR is diagnosed in about 25% to 50% of children with UTI, which can cause recurrence risk and renal scar [4], so continuous prophylactic antibiotic use or surgical correction through early detection of VUR has been considered necessary in all children with UTI.
AAP recommended VCUG in all first febrile UTIs in guidelines of 1999 [5], but follow-up studies showed that the use of continuous prophylactic antibiotics or surgical correction did not reduce renal scars [16-19] in children with VUR. In addition, it was virtually impossible completely prevent renal scar in children with VUR [20-24] because most of the severe renal scars that cause hypertension and chronic renal failure, occurred prior to infection from the fetal period. Therefore, questions have been raised about the role of VCUG implemented after the first febrile UTI, and the changed guidelines recommend selective implementation. The 2007 British guidelines recommended VCUG only in atypical UTIs that did not respond well to treatment or recurrent UTIs in infants less than 6 months [25]. They suggested that VCUG was not required in children with uncomplicated UTIs over 6 months of age. The 2011 revised guidelines of AAP recommended VCUG only for in children with abnormalities on USG, atypical clinical course, or children with recurrent UTI, and no longer for all children with first febrile UTI [6].
So, many researchers studies have been making efforts to find the predictor for VUR because of the invasiveness, and the risk of radiation exposure VCUG. Oostenbrink et al. [7] suggested male, younger age, family history of urinary tract diseases, high level of CRP, and abnormal findings of USG findings as independent factors of VUR. The authors aimed to identify the value of DNI in predicting the presence of VUR in children with febrile UTIs. Recently, Lee et al. [15] have identified the value of DNI with a comprehensive and more detailed study. In contrast, our study is a single institutional study and does not include dimercaptosuccinic acid (DMSA) scan. However, we verified that DNI was still worth predicting the presence of VUR even when the child with UTI is older than 12 months of age.
Our study confirmed that DNI and ultrasonography were predictors of VUR, which showed similar results to previous studies by Lee et al. [15] Especially, the area under the curve value of DNI in the ROC curve was the highest, so it was found to be more useful as VUR predictor than the finding of USG-positive recommended by most guidelines.
The cutoff value, which can predict VUR, was set at 1.85, which is low in usefulness as a screening test due to its sensitivity at 68.2%. However, the negative predictive value is very high at 93.4%. It means the following facts; if the value of DNI is less than 1.85 in children with UTI, it is highly unlikely that VUR will be present. In this study, the DNI cutoff value was lower than that in other studies such as sepsis, which is thought to be because febrile UTI belongs to mild diseases compared to severe infectious diseases such as sepsis. The mean value of all patients in this study was 0.3 (┬▒6.4). Previously, the value of DNI more than 6.5% was a significant indicator of sepsis or septic shock [26].
Contrary to most studies suggesting male sex as predictors of VUR, we found that boys had a lower risk of OR (0.348; 95% CI, 0.157ŌĆō0.774), which seems unlikely to have a significant difference in sex between the group with and without VUR (P=0.158).
Our study has a few practical limitations. Above all, the subjects of the study are patients from the past. That is the limitation of this research being conducted retrospectively. Since 2011, VCUG was undertaken selectively. If the subjects were selected as recent patients, the selection bias would be significant. Also, there may be bias in patients whose DNI values are not measured or who have not undergone kidney USG or VCUG. Because it is a single institutional study, the number of data is relatively small and did not include the duration of fever or family history, which has been considered important in previous studies. In addition, we have not been able to compare DNI index with other reliable tools for VUR prediction, such as DMSA scan and urinary neutrophil gelatinase-associated lipocalin (NGAL). Traditionally, DMSA scan can find the possibility of a VUR very sensitively by finding a renal scar. However, there is a risk of radiation, and sedation for children of younger age. Recently, NGAL has been reported as a rapid and noninvasive method in the diagnosis of VUR [27]. Urinary NGAL-creatinine ratio is higher in children with VUR and may be used as a rapid and noninvasive method in diagnosing VUR. It is a sensitive and specific biomarker, but it still needs additional laboratory testing, and it is not covered by national health insurance.
Our study confirmed the usefulness of DNI as a predictor of VUR and also found that it was a better index than USG-positive, which was previously used as the best screening tool for VUR. We suggest that if the DNI value is lower than the cutoff, VCUG can be withheld because the negative predictive value of DNI is very high in children with febrile UTI. However, as previously described, since this study was conducted retrospectively in a single institution, additional large-scale prospective studies would be needed.
Notes
Ethical statements
This study protocol was approved by Institutional Review Boards (IRB) of Konyang University Hospital (No. KYUH 2021-01-013-001). We were given exemption from getting informed consents by the IRB because the present study was a retrospective study, personal identifiers were completely removed, and the data were analyzed anonymously. Our study was conducted according to the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Author contributions
Conceptualization: JEK, JSO, JMY, KOK, EJC
Data curation: JEK, JSO, JMY, KOK, EJC
Formal analysis: JEK, JSO, JMY, KOK, EJC
Investigation: JEK, JSO, JMY, KOK, EJC
Methodology: JEK, JSO, JMY, KOK, EJC
Project administration: JEK, EJC
Visualization: JEK, JSO, JMY, KOK, EJC
Writing-original draft: JEK, JSO, JMY, KOK, EJC
Writing-review & editing: JEK, JSO, JMY, KOK, EJC
All authors read and approved the final manuscript.
References
1. Jacobson SH, Eklof O, Lins LE, Wikstad I, Winberg J. Long-term prognosis of post-infectious renal scarring in relation to radiological findings in childhood: a 27-year follow-up. Pediatr Nephrol 1992;6:19-24.



2. Montini G, Tullus K, Hewitt I. Febrile urinary tract infections in children. N Engl J Med 2011;365:239-50.


3. Ginsburg CM, McCracken GH Jr. Urinary tract infections in young infants. Pediatrics 1982;69:409-12.



4. Yilmaz S, Ozcakar ZB, Kurt Sukur ED, Bulum B, Kavaz A, Elhan AH, et al. Vesicoureteral reflux and renal scarring risk in children after the first febrile urinary tract infection. Nephron 2016;132:175-80.


5. American Academy of Pediatrics. Committee on Quality Improvement. Subcommittee on Urinary Tract Infection. Practice parameter: the diagnosis, treatment, and evaluation of the initial urinary tract infection in febrile infants and young children. Pediatrics 1999;103(4 Pt 1):843-52.


6. Subcommittee on Urinary Tract Infection, Steering Committee on Quality Improvement and Management; Roberts KB. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics 2011;128:595-610.



7. Oostenbrink R, van der Heijden AJ, Moons KG, Moll HA. Prediction of vesico-ureteric reflux in childhood urinary tract infection: a multivariate approach. Acta Paediatr 2000;89:806-10.


8. Choi EJ, Lee MJ, Park SA, Lee OK. Predictors of high-grade vesicoureteral reflux in children with febrile urinary tract infections. Child Kidney Dis 2017;21:136-41.

9. Nahm CH, Choi JW, Lee J. Delta neutrophil index in automated immature granulocyte counts for assessing disease severity of patients with sepsis. Ann Clin Lab Sci 2008;38:241-6.

10. Ansari-Lari MA, Kickler TS, Borowitz MJ. Immature granulocyte measurement using the Sysmex XE-2100. Relationship to infection and sepsis. Am J Clin Pathol 2003;120:795-9.


11. Mare TA, Treacher DF, Shankar-Hari M, Beale R, Lewis SM, Chambers DJ, et al. The diagnostic and prognostic significance of monitoring blood levels of immature neutrophils in patients with systemic inflammation. Crit Care 2015;19:57.




12. Harris N, Kunicka J, Kratz A. The ADVIA 2120 hematology system: flow cytometry-based analysis of blood and body fluids in the routine hematology laboratory. Lab Hematol 2005;11:47-61.

13. Lee SH, Ko KO, Lim JW, Yoon JM, Song YH, Lee JW, et al. Delta-neutrophil index: a potential predictor of coronary artery involvement in Kawasaki disease by retrospective analysis. Rheumatol Int 2019;39:1955-60.



14. Koh ID, Jeon IS, Kim HM. Diagnostic significance of the delta neutrophil index and other conventional parameters in neonatal bacteremia. Pediatr Infect Vaccine 2017;24:1-6.


15. Lee JW, Kim SH, Park SJ, Lee KH, Park JH, Kronbichler A, et al. The value of delta neutrophil index in young infants with febrile urinary tract infection. Sci Rep 2017;7:41265.




16. Keren R, Carpenter MA, Hoberman A, Shaikh N, Matoo TK, Chesney RW, et al. Rationale and design issues of the Randomized Intervention for Children With Vesicoureteral Reflux (RIVUR) study. Pediatrics 2008;122 Suppl 5(Suppl 5):S240-50.




17. Montini G, Rigon L, Zucchetta P, Fregonese F, Toffolo A, Gobber D, et al. Prophylaxis after first febrile urinary tract infection in children? A multicenter, randomized, controlled, noninferiority trial. Pediatrics 2008;122:1064-71.



18. Pennesi M, Travan L, Peratoner L, Bordugo A, Cattaneo A, Ronfani L, et al. Is antibiotic prophylaxis in children with vesicoureteral reflux effective in preventing pyelonephritis and renal scars? A randomized, controlled trial. Pediatrics 2008;121:e1489-94.



19. Hodson EM, Wheeler DM, Vimalchandra D, Smith GH, Craig JC. Interventions for primary vesicoureteric reflux. Cochrane Database Syst Rev 2007;(3):CD001532.


20. Koyle MA, Elder JS, Skoog SJ, Mattoo TK, Pohl HG, Reddy PP, et al. Febrile urinary tract infection, vesicoureteral reflux, and renal scarring: current controversies in approach to evaluation. Pediatr Surg Int 2011;27:337-46.



21. Lim R. Vesicoureteral reflux and urinary tract infection: evolving practices and current controversies in pediatric imaging. AJR Am J Roentgenol 2009;192:1197-208.


22. Merguerian PA, Sverrisson EF, Herz DB, McQuiston LT. Urinary tract infections in children: recommendations for antibiotic prophylaxis and evaluation: an evidence-based approach. Curr Urol Rep 2010;11:98-108.



23. Riccabona M, Avni FE, Blickman JG, Dacher JN, Darge K, Lobo ML, et al. Imaging recommendations in paediatric uroradiology: minutes of the ESPR workgroup session on urinary tract infection, fetal hydronephrosis, urinary tract ultrasonography and voiding cystourethrography, Barcelona, Spain, June 2007. Pediatr Radiol 2008;38:138-45.



24. Williams GJ, Hodson EH, Isaacs D, Craig JC. Diagnosis and management of urinary tract infection in children. J Paediatr Child Health 2012;48:296-301.

25. National Collaborating Centre for Women's and Children's Health. Urinary tract infection in children: diagnosis, treatment and long-term management. London: RCOG Press; 2007.
Fig.┬Ā2.
Receiver operating curve for predicting vesicoureteral reflux. CRP, C-reactive protein; DNI, delta neutrophil index.
Table┬Ā1.
Baseline characteristics of children in VUR positive or negative groups
Table┬Ā2.
Multivariable logistic regression analysis of clinical and laboratory parameters for prediction of vesicoureteral reflux
- TOOLS
-
 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link XML Download
XML Download Full text via DOI
Full text via DOI-
 Download Citation
Download Citation
- Download Citation
-
- Close
 Print
Print-
Share :



-
METRICS

-
- 0 Crossref
- 0 Scopus
- 2,346 View
- 48 Download
- ORCID iDs
-
Jae Eun Kim

https://orcid.org/0000-0001-6287-4342Jun Suk Oh

https://orcid.org/0000-0002-5765-2347Jung Min Yoon

https://orcid.org/0000-0003-3496-0061Kyung Ok Ko

https://orcid.org/0000-0003-4407-9534Eun Jung Cheon

https://orcid.org/0000-0003-3844-0864 - Related articles