| Child Kidney Dis > Volume 27(2); 2023 > Article |
|
Abstract
Renal nutcracker syndrome (NCS) is the entrapment of the left renal vein between the abdominal aorta and superior mesenteric artery. Although uncommon in pediatric patients, early diagnosis is crucial to avoid potential severe complications, such as anemia or renal vein thrombosis. NCS presents a variety of symptoms, most commonly including ŌĆ£TriadeŌĆÖs symptomsŌĆØŌĆōhematuria, proteinuria, and flank pain. Diagnosis and treatment include invasive and noninvasive management, although due to a lack of pediatric clinical studies, management is widely variable. Conservative diagnosis and treatment are recommended as a first-line option for pediatric patients; however, invasive surgical treatment may be recommended based on symptom severity. This review aims to provide a comprehensive overview of NCS in children to better understand the widely variable incidence, occurrence, and management from early on to allow for early-onset management.
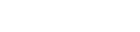
Renal nutcracker syndrome (NCS) is a rare pediatric disease that is defined as the symptomatic entrapment of the left renal vein (LRV). In the anterior form, the LRV is compressed between the aorta and mesenteric artery (Fig. 1), or less commonly between the aorta and vertebral column, known as posterior NCS. Common symptoms include hematuria, proteinuria, and flank pain, known as ŌĆ£TriadeŌĆÖs symptoms,ŌĆØ although there is still wide variability in clinical presentation among children [1-3]. Symptoms are believed to result from increased pressure within the renal vein and the kidneyŌĆÖs venous drainage system. This elevated pressure is believed to harm the thin-walled septa between the veins and the collecting system in the renal fornix, leading to hematuria or proteinuria [2]. However, pathological evidence supporting this hypothesis is still lacking [4].
Although the terms ŌĆ£nutcracker phenomenon (NCP)ŌĆØ and ŌĆ£NCSŌĆØ were used interchangeably in earlier literature, NCP specifically refers to the anatomical structure without the occurrence of symptoms [1,4,5]. The first pathological description of this anatomical structure was attributed to the anatomist Grant in 1937 [1], following the first clinical report of the phenomenon by El-Sadr and Mina in 1950 [6]. The term ŌĆ£NCSŌĆØ is commonly attributed to the Belgian physician de Schepper [7], although it was initially used by Chait et al. in 1971 [8].
While there is extensive research on NCS in adults [2,4], the incidence, diagnostic criteria, and treatment remain undefined in the pediatric cohort due to its rarity in children [9]. The exact incidence of NCS in children remains unknown [4]; however, a peak age period of diagnosis was observed between ages 10 and 14 years [10,11]. Timely identification of NCS is crucial due to the potential occurrence of more severe complications such as severe anemia or renal vein thrombosis resulting from hematuria [12]. Given the wide variability of NCS in the pediatric population, this literature review aimed to provide a better comprehensive understanding and overview of the disease in children.
A wide range of symptoms has been observed in children with NCS due to the varying hemodynamic consequences of LRV compression [13]. LRV compression raises the retrograde venous pressure, impacting other associated vessels and leading to various clinical manifestations [14].
The most common symptoms observed in children with NCS are hematuria (micro- and macrohematuria), proteinuria (mainly orthostatic), and flank pain [3,5,9,13,15]. Additional studies observed symptoms such as renovascular hypertension, unspecified abdominal pain, dysmenorrhea, nephrolithiasis, calciuria, fatigue, testicular or scrotal pain, and varicocele [3,11,16,17]. Symptoms also often worsen with physical exercise [2,3].
Hematuria is the most frequently observed symptom in pediatric patients [3,7,18], occurring due to increased venous pressure leading to varicose veins rupturing and consequently bleeding into the renal collecting system [9,16]. Hematuria has been reported as the most frequent symptom in 75% of pediatric patients with NCS [3]. Children often experience microscopic hematuria asymptomatically, compared to adults, who more often experience hematuria with pain [11]. Additionally, a systematic review on pediatric NCS analyzing published literature from 1990 to 2020 described hematuria as the most commonly experienced symptom, observed in approximately 55% of children with NCS. This was followed by proteinuria and flank pain, observed in approximately 50% and 19% of children, respectively [9].
Although NCS can develop in individuals of all age groups, a higher incidence is observed in underweight or lean children aged 10 to 14 years, with a slight prevalence among females [14]. In a systematic review assessing 423 children with NCS (218 males and 205 females), the mean age of the study participants was 12 years [9].
Due to the rarity of NCS in children and a limited number of published studies, standardized diagnostic criteria for NCS in pediatric patients are lacking. Diagnosis often relies on exclusion criteria and utilizes conservative and invasive techniques [19].
In adults, renal venography is the first-line diagnostic examination [20,21]; other standard diagnostic techniques include renal Doppler ultrasonography (USG), magnetic resonance angiography, computed tomography (CT), and multislice helical CT angiography [22-25]. In contrast, many noninvasive diagnostic techniques, such as Doppler USG, magnetic resonance imaging (MRI), or CT, are initially recommended for children [26-28]. As varicocele is often observed simultaneously with NCS in approximately 33% of male pediatric patients, Doppler USG is further recognized as an effective diagnostic technique [3]. Additionally, urinalysis helps identify potential NCS manifestations, including repeated hematuria (gross or microscopic), calciuria, and orthostatic proteinuria [9,29].
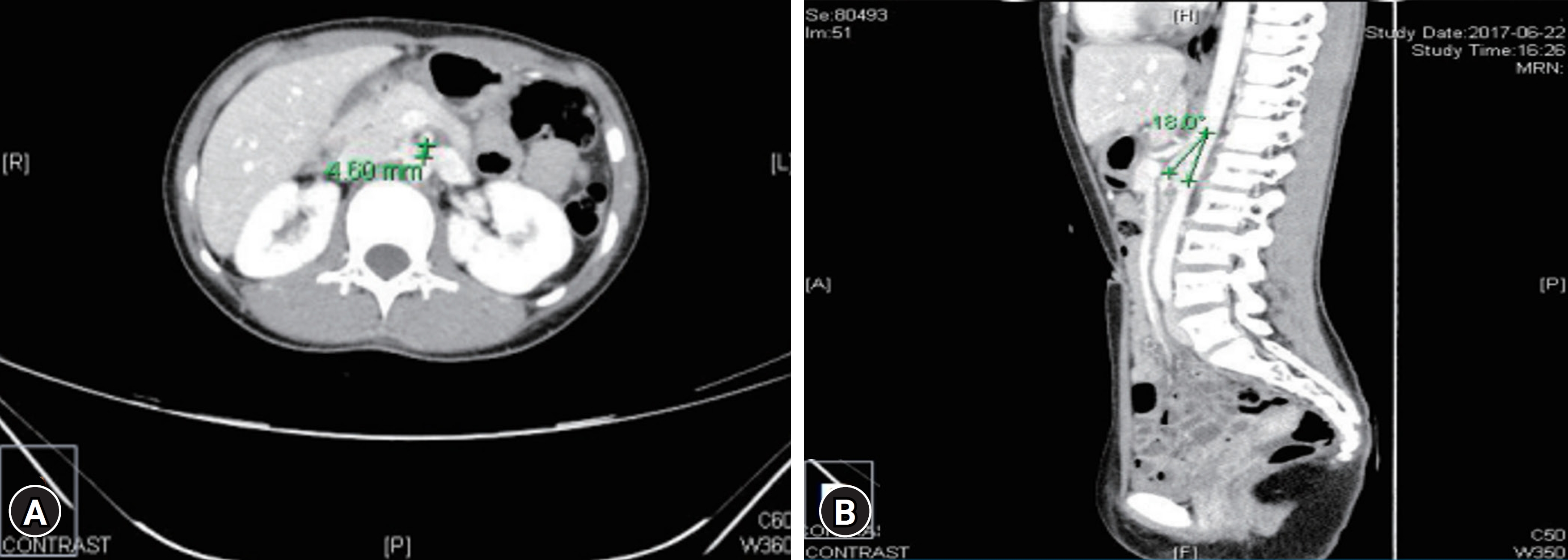
In children, recommended noninvasive examinations such as abdominal USG and Doppler studies are reported to have a sensitivity and specificity of approximately 82.3% and 89%ŌĆō100%, respectively [3]. In the general population of patients with NCS, an aortomesenteric (AOM) angle of <35┬░ is significantly characteristic of diagnosis (Figs. 2, 3) [30]. A previous study involving 205 pediatric patients reported an AOM angle of <25┬░ in approximately 9% of asymptomatic pediatric patients with NCS [31]. Additionally, a study including 39 pediatric patients with orthostatic proteinuria reported that a ratio greater than 0.6 between the AOM angle in the upright and supine positions could be diagnostic of NCS [32]. However, additional criteria and further studies are required to validate the exact cutoff angle [20,33].
The diameter of LRV and peak velocity ratio in the AOM and hilar portions can also serve as diagnostic criteria for NCS in children (Figs. 2, 3) [3,9]. According to a study in 2002, a ratio greater than 4.2 for the diameter of LRV and 4.0 for the peak velocity ratio can be used as cutoff values to diagnose NCS [22]. A study enrolling a group of 12 pediatric patients published in 2006 recommended a peak velocity cutoff value of 4.7 (with specificity of 90% and sensitivity of 100%) [23]. Consequently, a study in 2007 including 216 pediatric patients with isolated hematuria that reported NCS in approximately 33% of patients recommended a peak velocity ratio of at least 4.1 [24]. These varying results highlight the need for further research to validate peak velocity or LRV ratio cutoff values in diagnosing NCS.
Although conservative techniques are often recommended for diagnosis, invasive diagnostic techniques such as intravascular USG or phlebography are performed under circumstantial cases to assess the obstruction severity [9,28,29]. These invasive techniques may involve catheterization to measure the pressure gradient between the inferior vena cava (IVC) and LRV. The typical pressure gradient between IVC and LRV in the general population is <1 mmHg [28]. When the pressure gradient exceeds 3 mmHg, a definitive diagnosis of NCS is established [21,25,28]. Renal biopsies, venography, arteriography, cystoscopy, and intravenous urography are additional invasive techniques used in children [9].
Comorbidities frequently observed in pediatric patients with NCS include varicocele, chronic fatigue syndrome or idiopathic chronic fatigue, superior mesenteric artery (SMA) syndrome, and WilkieŌĆÖs syndrome [34-39]. Table 1 describes the comorbidities observed in pediatric patients with NCS from previously published studies.
Varicocele is characterized by the enlargement of veins within the scrotum and exhibits a direct association with NCS in male children [34]. In cases where NCS is present, it can contribute to the development or exacerbation of varicocele [40]. A study involving 3,042 patients with varicocele, including 858 LRV entrapment cases, reported a risk ratio of 43.3 for LRV entrapment-associated varicocele recurrence [34].
Furthermore, occasional associations have been observed between chronic fatigue syndrome and NCS, characterized by elevated LRV-IVC pressure gradients. Fatigue symptoms have shown a positive correlation with high peak velocity ratios through Doppler USG; in some instances, these symptoms have improved postoperatively [41-43]. This association was also reported in a study that observed nine pediatric patients with severe NCP and chronic fatigue syndrome or chronic fatigue [35]. Additionally, two case studies have reported the coexistence of NCS with SMA syndrome in a 15-year-old male and a 14-year-old female [36,37]. WilkieŌĆÖs syndrome has also been recorded to occur concurrently with NCS in two case studies with 15-year-old and 17-year-old males [38,39].
Additional complications unrelated to NCS but observed in pediatric patients with NCS include immunoglobulin A nephropathy, immunoglobulin M nephropathy, intussusception, Henoch-Sch├Čnlein purpura, right retrocaval ureter, urolithiasis, LRV duplication, renal abscess, midline congestion syndrome, celiacomesenteric trunk anomaly, intestinal malrotation, and spontaneous spermatic vein thrombosis [44-55].
Two main treatment approaches for NCS include conservative and surgical treatments. In adults, surgical treatment is often considered the initial therapy of choice. Conversely, in pediatric patients, a conservative approach, often involving a watch-and-wait strategy, is typically recommended for a minimum duration of 2 years [40,56,57]. The choice between conservative and nonconservative management is controversial and often depends on the clinical status and severity of symptoms [58].
The recommendation for conservative management in children is supported by previous studies that have demonstrated the spontaneous resolution of symptoms as children undergo physical development. According to a comprehensive systematic review, out of 138 pediatric patients who received conservative treatment for NCS, approximately 95% achieved complete resolution or symptom improvement (43% or 52%, respectively) [9]. Regarding hematuria in pediatric patients with NCS, after a mean follow-up of 1.5 years, 75% of pediatric patients experienced a complete resolution of hematuria. This study also recorded a significant increase in patient height and weight and a significant decrease in LRV and peak velocity ratios, suggesting how body mass index (BMI) may be a potential hemodynamic factor for the spontaneous resolution of hematuria [59].
Although the exact mechanism behind the spontaneous resolution of symptoms remains unclear, adolescent growth and an increase in BMI may be indicators for the prognosis of NCS. A study involving 23 children with NCS showed a significant correlation between BMI and the regression of hematuria and proteinuria symptoms. The study reported an initial average BMI of 16.9 kg/m2, significantly increasing to 18.6 kg/m2 during the follow-up period [16]. An increase in body weight in adolescents often modifies the position of the left kidney, allowing for a decrease in pressure on the LRV [4,16]. Additionally, the physical growth of the patient can prompt fibrous tissue proliferation at the origin of the SMA, partially relieving the compression at the AOM angle [40].
Although conservative treatment is highly recommended, when severe NCS symptoms persist, various surgical and endovascular treatments techniques may be applied. Common surgical treatments include the LRV, SMA, or left gonadal vein transposition, kidney autotransplantation, endovascular stent placement, laparoscopy, and shunt operation [60-65]. Among them, LRV transposition is considered the gold standard surgical treatment for uncompensated NCS. Other surgical options depend on the patientŌĆÖs specific case and context, such as symptoms severity, stage of the syndrome, and patient age [9,66]. For example, in a cohort of 53 male pediatric patients diagnosed with NCS and varicocele, spermatic-inferior epigastric vein anastomosis was performed. Approximately 96% and 49% of patients experienced improved NCS and scrotal bulge symptoms postoperatively [67]. Another example of case-specific operative treatment was recorded in managing NCS in a 16-year-old female. In situ, gonadal vein valvotomy and side-to-side gonado-iliac bypass were performed, resulting in a complete resolution in the patient [68]. Furthermore, in a case study of a 14-year-old female with NCS, orthostatic proteinuria resolved after angiotensin-converting enzyme inhibition therapy, although this treatment may affect renal hemodynamics in children [15,69].
In summary, NCS treatment varies depending on the patientŌĆÖs specific context. However, further clinical studies with long-term follow-up are required to evaluate the effectiveness of different treatment approaches.
Early diagnosis of NCS is crucial to prevent severe complications such as anemia or renal vein thrombosis. NCS symptoms vary widely, including hematuria, proteinuria, and flank pain. Due to pediatric NCSŌĆÖs rarity, diagnostic criteria are not well-established, although common noninvasive diagnostic techniques include Doppler USG, MRI, and CT for initial diagnosis. Comorbidities associated with NCS in pediatric patients include chronic fatigue syndrome, chronic fatigue, varicocele, SMA syndrome, and WilkieŌĆÖs syndrome. Treatment options for NCS range from conservative management to surgical interventions. Further research and clinical studies with long-term follow-up are necessary to establish standardized diagnostic criteria and evaluate the efficacy of different treatment approaches for NCS in pediatric patients. These studies should additionally focus on evaluating the accuracy of noninvasive techniques, exploring the impact of associated comorbidities, and assessing the efficacy and safety of different treatment approaches. A better understanding of NCS in children will enable early management and improved outcomes.
Notes
Conflicts of interest
Se Jin Park and Jae IL Shin are editorial board members of the journal but were not involved in the peer reviewer selection, evaluation, and decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Author contributions
Conceptualization: DSK, JIS
Data curations: DSK, SJP
Formal analysis: DSK, SJP, JIS
Investigation: DSK, SJP
Methodology: DSK, SJP, JIS
Project administration: SJP, JIS
Visualization: DSK, SJP
Writing-original draft: DSK, SJP
Writing-review & editing: DSK, SJP, JIS
All authors read and approved the final manuscript.
References
1. Kolber MK, Cui Z, Chen CK, Habibollahi P, Kalva SP. Nutcracker syndrome: diagnosis and therapy. Cardiovasc Diagn Ther 2021;11:1140-9.


2. Kurklinsky AK, Rooke TW. Nutcracker phenomenon and nutcracker syndrome. Mayo Clin Proc 2010;85:552-9.



3. Miro I, Serrano A, Perez-Ardavin J, March JA, Polo A, Conca MA, et al. Eighteen years of experience with pediatric nutcracker syndrome: the importance of the conservative approach. J Pediatr Urol 2020;16:218.


4. Granata A, Distefano G, Sturiale A, Figuera M, Foti PV, Palmucci S, et al. From nutcracker phenomenon to nutcracker syndrome: a pictorial review. Diagnostics (Basel) 2021;11:101.



5. Agarwal A, Litra F, Barr LL. A rare cause of abdominal and flank pain in children: nutcracker syndrome. Cureus 2021;13:e16422.



6. El-Sadr AR, Mina E. Anatomical and surgical aspects in the operative management of varicocele. Urol Cutaneous Rev 1950;54:257-62.

7. de Schepper A. "Nutcracker" phenomenon of the renal vein and venous pathology of the left kidney. J Belge Radiol 1972;55:507-11.

8. Chait A, Matasar KW, Fabian CE, Mellins HZ. Vascular impressions on the ureters. Am J Roentgenol Radium Ther Nucl Med 1971;111:729-49.


9. Meyer J, Rother U, Stehr M, Meyer A. Nutcracker syndrome in children: appearance, diagnostics, and treatment: a systematic review. J Pediatr Surg 2022;57:716-22.


10. Mallat F, Hmida W, Othmen MB, Mosbah F. Mixed nutcracker syndrome with left renal vein duplication: a severe and exceptional presentation in an 18-year-old boy. Urol Ann 2015;7:244-7.



11. Vianello FA, Mazzoni MB, Peeters GG, Fossali EF, Camozzi P, Bianchetti MG, et al. Micro- and macroscopic hematuria caused by renal vein entrapment: systematic review of the literature. Pediatr Nephrol 2016;31:175-84.



12. Oteki T, Nagase S, Hirayama A, Sugimoto H, Hirayama K, Hattori K, et al. Nutcracker syndrome associated with severe anemia and mild proteinuria. Clin Nephrol 2004;62:62-5.


13. Basaran EG, Yilmaz AC, Gungor O, Tayfur AC, Buyukkaragoz B. Clinical profile and renal ultrasound characteristics of children with nutcracker syndrome in Turkey. Indian Pediatr 2022;59:28-30.



14. Reddy DK, Shekar P A. Nutcracker syndrome: a rare but important cause of varicocele in adolescent boys. Urology 2020;141:143-6.


15. Shin JI, Lee JS. ACE inhibition in nutcracker syndrome with orthostatic proteinuria: how about a hemodynamic effect? Pediatr Nephrol 2007;22:758-60.


16. Alaygut D, Bayram M, Soylu A, Cakmakci H, Turkmen M, Kavukcu S. Clinical course of children with nutcracker syndrome. Urology 2013;82:686-90.


17. Mazzoni MB, Kottanatu L, Simonetti GD, Ragazzi M, Bianchetti MG, Fossali EF, et al. Renal vein obstruction and orthostatic proteinuria: a review. Nephrol Dial Transplant 2011;26:562-5.


18. Li H, Sun X, Liu G, Zhang Y, Chu J, Deng C, et al. Endovascular stent placement for nutcracker phenomenon. J Xray Sci Technol 2013;21:95-102.


19. Jiang Y, Gan Z, Wang Q, Chen Y, Jiang Y. Bibliometric and visual analysis of research on nutcracker syndrome from 1974 to 2021: a systematic review. Medicine (Baltimore) 2022;101:e29939.



20. Park SJ, Shin JI. Comment on: nutcracker and SMA syndromes: what is the normal SMA angle in children? (Eur J Radiol. 2012;81(August (8)):e854-61). Eur J Radiol 2013;82:1034.


21. Beinart C, Sniderman KW, Tamura S, Vaughan ED, Sos TA. Left renal vein to inferior vena cava pressure relationship in humans. J Urol 1982;127:1070-1.


22. Park SJ, Lim JW, Cho BS, Yoon TY, Oh JH. Nutcracker syndrome in children with orthostatic proteinuria: diagnosis on the basis of Doppler sonography. J Ultrasound Med 2002;21:39-46.


23. Cheon JE, Kim WS, Kim IO, Kim SH, Yeon KM, Ha IS, et al. Nutcracker syndrome in children with gross haematuria: Doppler sonographic evaluation of the left renal vein. Pediatr Radiol 2006;36:682-6.



24. Shin JI, Park JM, Lee JS, Kim MJ. Effect of renal Doppler ultrasound on the detection of nutcracker syndrome in children with hematuria. Eur J Pediatr 2007;166:399-404.




25. Nishimura Y, Fushiki M, Yoshida M, Nakamura K, Imai M, Ono T, et al. Left renal vein hypertension in patients with left renal bleeding of unknown origin. Radiology 1986;160:663-7.


26. Kim SH, Cho SW, Kim HD, Chung JW, Park JH, Han MC. Nutcracker syndrome: diagnosis with Doppler US. Radiology 1996;198:93-7.


27. Atasoy D, Cansu A, Bekircavusoglu AF, Ozdogan EB, Ahmetoglu A. The utility of magnetic resonance angiography in children with nutcracker syndrome. Turk J Med Sci 2021;51:2396-402.



29. Ahmed K, Sampath R, Khan MS. Current trends in the diagnosis and management of renal nutcracker syndrome: a review. Eur J Vasc Endovasc Surg 2006;31:410-6.


30. Min KW, Lee OK, Kim MK. Nutcracker syndrome combined with superior mesenteric artery syndrome in a pediatric patient: a case report. Child Kidney Dis 2018;22:75-80.

31. Arthurs OJ, Mehta U, Set PA. Nutcracker and SMA syndromes: what is the normal SMA angle in children? Eur J Radiol 2012;81:e854-61.


32. Gulleroglu NB, Gulleroglu K, Uslu N, Baskin E. Left renal vein entrapment in postural proteinuria: the diagnostic utility of the aortomesenteric angle. Eur J Pediatr 2022;181:3339-43.



33. Fitoz S, Ekim M, Ozcakar ZB, Elhan AH, Yalcinkaya F. Nutcracker syndrome in children: the role of upright position examination and superior mesenteric artery angle measurement in the diagnosis. J Ultrasound Med 2007;26:573-80.


34. Li S, Liu Q, Wang J, Pang X, Zhang Y, Cheng Y, et al. Association between left renal vein entrapment and varicocele recurrence: a cohort study in 3042 patients. Sci Rep 2018;8:10534.




35. Takahashi Y, Ohta S, Sano A, Kuroda Y, Kaji Y, Matsuki M, et al. Does severe nutcracker phenomenon cause pediatric chronic fatigue? Clin Nephrol 2000;53:174-81.

36. Lin TH, Lin CC, Tsai JD. Superior mesenteric artery syndrome and nutcracker syndrome. Pediatr Neonatol 2020;61:351-2.


37. Du MC, Chen HY, Zhang YX, Zhang LB. Pica with superior mesenteric artery syndrome and nutcracker syndrome as imaging manifestation: a case report. Asian J Surg 2022;45:2038-9.


38. England J, Li N. Superior mesenteric artery syndrome: a review of the literature. J Am Coll Emerg Physicians Open 2021;2:e12454.




39. Gungorer V, Ozturk M, Arslan S. A rare cause of recurrent abdominal pain: the coexistence of Wilkie's syndrome and nutcracker syndrome. Arch Argent Pediatr 2023;121:e202102373.


40. Ananthan K, Onida S, Davies AH. Nutcracker syndrome: an update on current diagnostic criteria and management guidelines. Eur J Vasc Endovasc Surg 2017;53:886-94.


41. Stewart JM, Gewitz MH, Weldon A, Munoz J. Patterns of orthostatic intolerance: the orthostatic tachycardia syndrome and adolescent chronic fatigue. J Pediatr 1999;135:218-25.


42. Juhn JH, Yoo BW, Lee JS, Kim MJ. A case of nutcracker syndrome associated with orthostatic proteinuria and idiopathic chronic fatigue in a child. J Korean Soc Pediatr Nephrol 2001;5:64-8.
43. Shin JI, Lee JS. Can chronic fatigue symptoms associated with nutcracker phenomenon be treated with aspirin? Med Hypotheses 2007;69:704-5.


44. Shin JI, Park JM, Shin YH, Lee JS, Kim MJ, Jeong HJ. Nutcracker syndrome combined with IgA nephropathy in a child with recurrent hematuria. Pediatr Int 2006;48:324-6.


45. Strul N, Vaessen S, Collard L, Ghuysen MS, Khamis J, Brisbois D, et al. Clinical case of the month: nutcracker syndrome in association with a painful nephrologic disease. Rev Med Liege 2007;62:73-6.

46. Shin JI, Lee SM, Park JM, Shin YH, Lee JS, Kim MJ. Doppler ultrasonographic detection of nutcracker syndrome in a young child with intussusception: a case report. Acta Paediatr 2005;94:1510-3.


47. Shin JI, Park JM, Shin YH, Lee JS, Kim MJ. Superimposition of nutcracker syndrome in a haematuric child with Henoch-Sch├Čnlein purpura. Int J Clin Pract 2005;59:1472-5.


48. Rao J, Yang J, Liu Z, Wang L, Liu L, Yin Z, et al. Right retrocaval ureter and left nutcracker syndrome: a case report. Urology 2008;71:1226.


49. Altugan FS, Ekim M, Fitoz S, Ozcakar ZB, Burgu B, Yalcinkaya F, et al. Nutcracker syndrome with urolithiasis. J Pediatr Urol 2010;6:519-21.


50. Preza Fernandes J, Amorim R, Gomes MJ, Oliveira V, Reis A, Ribeiro-Castro J. Posterior nutcracker syndrome with left renal vein duplication: a rare cause of haematuria in a 12-year-old boy. Case Rep Urol 2012;2012:849681.



51. Yavuz S, Ece A, Corapli M, Ilter C, Guven R. Nutcracker syndrome complicating with renal abscess. J Pak Med Assoc 2016;66:470-2.

52. Scholbach T. From the nutcracker-phenomenon of the left renal vein to the midline congestion syndrome as a cause of migraine, headache, back and abdominal pain and functional disorders of pelvic organs. Med Hypotheses 2007;68:1318-27.


53. Al-Zoubi NA, Al-Ghalayini IF, Al-Okour R. Nutcracker syndrome associated with celiacomesentric trunk anomaly: case report. Int J Nephrol Renovasc Dis 2017;10:285-8.




54. Nishio Y, Kawano Y, Hara S. Nutcracker syndrome complicated with intestinal malrotation. BMJ Case Rep 2019;12:e231230.



55. Perez-Ardavin J, Serrano Durba A, Miro I, Conca Baena MA, March-Villalba JA, Polo Rodrigo A, et al. Spontaneous spermatic vein thrombosis in pediatric patients: a condition to be considered. Cir Pediatr 2020;33:99-101.

56. Chang CT, Hung CC, Ng KK, Yen TH. Nutcracker syndrome and left unilateral haematuria. Nephrol Dial Transplant 2005;20:460-1.


57. Zhang H, Li M, Jin W, San P, Xu P, Pan S. The left renal entrapment syndrome: diagnosis and treatment. Ann Vasc Surg 2007;21:198-203.


58. Velasquez CA, Saeyeldin A, Zafar MA, Brownstein AJ, Erben Y. A systematic review on management of nutcracker syndrome. J Vasc Surg Venous Lymphat Disord 2018;6:271-8.


59. Shin JI, Park JM, Lee SM, Shin YH, Kim JH, Lee JS, et al. Factors affecting spontaneous resolution of hematuria in childhood nutcracker syndrome. Pediatr Nephrol 2005;20:609-13.



60. Reed NR, Kalra M, Bower TC, Vrtiska TJ, Ricotta JJ, Gloviczki P. Left renal vein transposition for nutcracker syndrome. J Vasc Surg 2009;49:386-94.


61. Chuang CK, Chu SH, Lai PC. The nutcracker syndrome managed by autotransplantation. J Urol 1997;157:1833-4.

62. Xu D, Liu Y, Gao Y, Zhang L, Wang J, Che J, et al. Management of renal nutcracker syndrome by retroperitoneal laparoscopic nephrectomy with ex vivo autograft repair and autotransplantation: a case report and review of the literature. J Med Case Rep 2009;3:82.




63. Thompson PN, Darling RC, Chang BB, Shah DM, Leather RP. A case of nutcracker syndrome: treatment by mesoaortic transposition. J Vasc Surg 1992;16:663-5.


64. Benrashid E, Turley RS, Mureebe L, Shortell CK. Gonadal vein transposition in the treatment of nutcracker syndrome. J Vasc Surg 2016;64:845.

65. Shaper KR, Jackson JE, Williams G. The nutcracker syndrome: an uncommon cause of haematuria. Br J Urol 1994;74:144-6.


66. de Macedo GL, Dos Santos MA, Sarris AB, Gomes RZ. Diagnosis and treatment of the nutcracker syndrome: a review of the last 10 years. J Vasc Bras 2018;17:220-8.



67. Hao J, Shi H, Xu H, Zhu J, Zhou J, Du T. Ultrasound-assisted microsurgical left spermatic-inferior epigastric vein anastomosis for treating nutcracker syndrome-associated varicocele. Int Urol Nephrol 2019;51:1925-32.



Fig.┬Ā1.
Illustration of renal nutcracker syndrome, depicting the compression of the LRV between the abdominal aorta and the SMA. LRA, left renal artery; LRV, left renal vein; SMA, superior mesenteric artery.
Fig.┬Ā2.
Images of Doppler ultrasonography. (A) The diameters of left renal vein in the aortomesenteric portion (0.13 cm) and the hilar portion (0.69 cm). (B) The peak velocity in the aortomesenteric portion (95 cm/sec). (C) The peak velocity in the hilar portion (18 cm/sec). (D) The aortomesenteric angle (18┬░). Reused from Min et al. Child Kidney Dis 2018;22:75-80 [30].
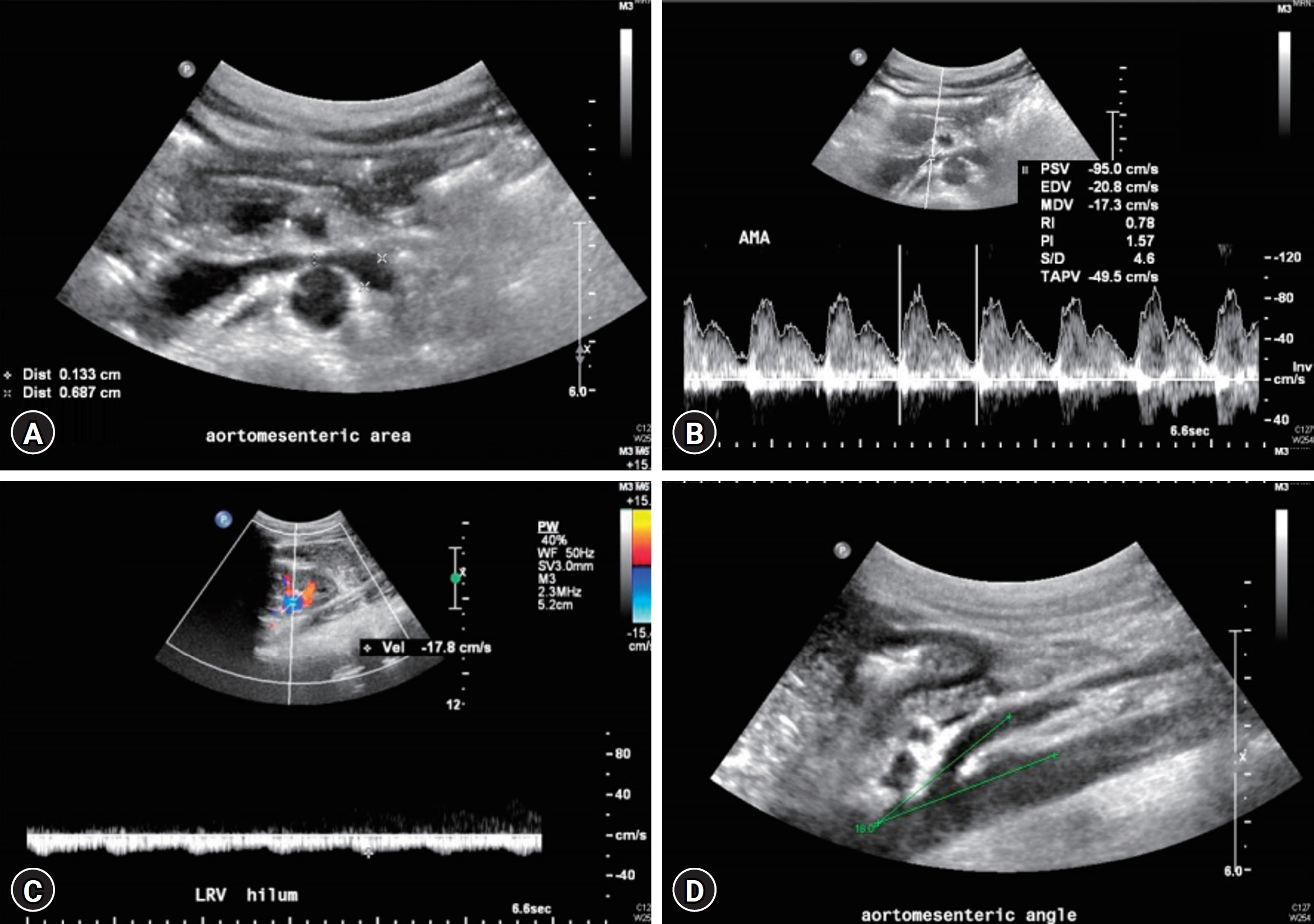
Fig.┬Ā3.
Abdomen and pelvis computed tomography (enhancement). (A) Left renal vein was compressed by the aorta and the superior mesenteric artery (aorto-superior mesenteric artery distance: 4.6 mm). (B) Aortomesenteric angle was 18┬░ in the sagittal plane. Reused from Min et al. Child Kidney Dis 2018;22:75-80 [30].
Table┬Ā1.
Comorbidities observed in pediatric patients with nutcracker syndrome
| Comorbidity | Author (year) | Patient characteristics |
|---|---|---|
| CFS, CF | Takahashi et al. (2000) [35] | 9 NCS children |
| Varicocele | Li et al. (2018) [34] | 858 NCS and 2,184 control |
| Reddy et al. (2020) [14] | 13-year-old boy | |
| SMA syndrome | Lin et al. (2020) [36] | 15-year-old male |
| Du et al. (2022) [37] | 14-year-old female | |
| WilkieŌĆÖs syndrome | England and Li (2021) [38] | 15-year-old male |
| Gungorer et al. (2022) [39] | 17-year-old male |
- TOOLS
-
 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link XML Download
XML Download Full text via DOI
Full text via DOI-
 Download Citation
Download Citation
- Download Citation
-
- Close
 Print
Print-
Share :



-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,509 View
- 18 Download
- ORCID iDs
-
Diana S. Kalantar

https://orcid.org/0009-0009-2233-163XSe Jin Park

https://orcid.org/0000-0002-7650-5393Jae Il Shin

https://orcid.org/0000-0003-2326-1820 - Related articles