A 22-month-old Boy with Acute Glomerulonephritis Coexistent with Hemolytic Anemia and Idiopathic Thrombocytopenia
Article information
Abstract
Hemolytic anemia and thrombocytopenia are rare clinical manifestations of acute glomerulonephritis. Initially, in all such cases, a diagnosis of hemolytic uremic syndrome, thrombotic thrombocytopenic purpura, systemic lupus erythematosus, and amyloidosis should be ruled out. The presence of hemolytic anemia and thrombocytopenia is rare, but possible, in a case of acute poststreptococcal glomerulonephritis, and may result in delayed diagnosis or misdiagnosis. Correct and timely diagnosis would ensure adequate treatment in such patients. We report of a 22-month-old boy with acute glomerulonephritis coexistent with hemolytic anemia and idiopathic thrombocytopenia.
Introduction
Acute poststreptococcal glomerulonephritis (APSGN) is one of the most common glomerulonephritides that affect children in developing countries [1]. Initial clinical manifestations of APSGN are variable. It is characterized by abrupt onset of gross hematuria, proteinuria, edema, and hypertension one to three weeks after an episode of an upper respiratory tract infection or pyoderma [1]. A low serum complement C3 level during the acute stage, and an eventual full clinical recovery with normal laboratory findings, except for persistent microscopic hematuria, are pathognomonic of APSGN [2]. Atypical manifestations of APSGN, such as hemolytic anemia and thrombocytopenia, are rarely reported. We report of a 22-month-old boy with acute glomerulonephritis coexistent with hemolytic anemia and idiopathic thrombocytopenia.
Case report
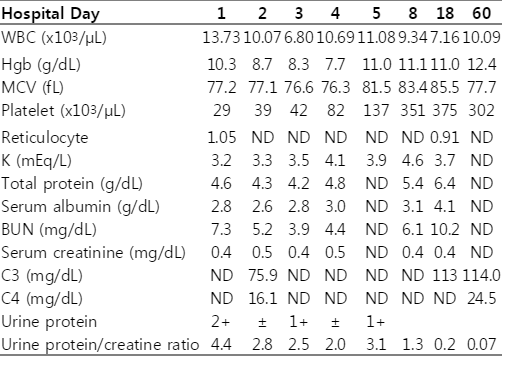
A 22-month-old boy was referred to our hospital with features of ischemic colitis, rectal prolapse, and sepsis. Five days before transfer to our hospital, he developed watery diarrhea, with a frequency of two times per day, along with mild fever and rhinorrhea. A day later, the frequency of watery diarrhea increased to twenty times per day despite antidiarrheal medications. Three days before transfer, he was admitted to a local hospital with complaints of blood-tinged diarrhea and poor oral intake. Laboratory findings revealed anemia (hemoglobin, 10.5 g/dL), thrombocytopenia (platelets, 43×103/µL), hypoalbuminemia (albumin, 2.6 g/dL), hypokalemia (potassium, 2.7 mmol/L), and proteinuria (1+ by dipstick exam). On the day of transfer, abdominal computed tomography (CT) was performed at the local hospital because the patient did not show any improvement. Abdominal CT revealed a water halo sign along with bowel wall edema and mucosal enhancement in the descending colon, sigmoid colon, and rectum. Ultimately, the patient was referred to our hospital. The medical history of the patient was insignificant. Except for eyelid swelling and diarrhea, there were no associated symptoms, such as fever, cough, rhinorrhea, nausea, vomiting, abdominal pain, headache, weight loss, edema, irritability, oliguria, or gross hematuria. At the time of admission, his vital signs were as follows: systolic blood pressure, 111 mm Hg; diastolic blood pressure, 63 mm Hg; heart rate, 121 beats/min; respiratory rate, 30 breaths/min; and body temperature, 36.8℃. His weight was 10.8 kg (10th percentile). The patient did not appear ill, had a clear mental status; the results of a clinical examination were unremarkable. Hematological findings were: hemoglobin, 10.3 g/dL; white blood cell count , 13,730/µL, with 47% segmented neutrophils, 36% lymphocytes, and 8% monocytes; platelet count, 29×103/µL; C-reactive protein, 111,000 µg/L; erythrocyte sedimentation rate, 15 mm/h; peripheral blood smear, microcytic normochromic, with schistocytes 1+ and acanthocytes 1+; reticulocyte count, 1.05%; total protein, 46 g/L; albumin, 2.8 g/dL; glucose, 5.3 mmol/L; blood urea nitrogen, 2.6 mmol urea/L; creatinine, 35.4 µmol/L; aspartate transaminase 44 U/L; alanine transaminase 12 U/L; total bilirubin, 10.3 µmol/L; lactate dehydrogenase, 1,702 U/L; sodium 137 mmol/L; potassium 3.2 mmol/L; chloride 107 mmol/L; total carbon dioxide 23.1 mmol/L; antistreptolysin O (ASO) titer, negative; prothrombin time (PT), 10.4 sec; activated partial thromboplastin time, 28.8 sec; fibrin degradation product >5 mg/L (reference range, negative); D-dimer, 5,054.7 µg/L (reference range, 68-494 µg/L); fibrinogen, 3.46 g/L (reference range, 2-4 g/L); antithrombin III, 92% (reference range, 80-120%); complement C3, 759 mg/L (reference range, 770-1,950 mg/ L); C4, 161 mg/L (reference range, 70-400 mg/L); cystatin C-based glomerular filtration rate, 123 mL/min/1.73m2; antineutrophil cytoplasmic antibody, negative; antinuclear antibody, negative; anti-double stranded-DNA antibody, negative; direct and indirect Coombs test, both negative; antiplatelet antibody, negative; iron, 13.1 µmol/L (reference range, 9-22 µmol/L); total iron-binding capacity, 30.07 µmol/L (reference range, 44.75-71.60 µmol/L); ferritin, 596.1 µg/L (reference range, 7-140 µg/L); and haptoglobin, <0.2 g/L (reference range, 0.22-1.64 g/L). Urinalysis revealed: specific gravity, 1.010; pH, 6.0; occult blood, 3+; protein, 2+; red blood cells (RBC), 31-50/high-power field (HPF); WBC, 1-4/HPF; and granular cast > 5/HPF; protein to creatinine ratio, 4.4; sodium, 47 mmol/L; potassium, 6.6 mmol/L; and osmolality, 243 mmol/Kg. Stool examination revealed the following: hemoglobin, 383 µg/L; WBC, not seen; rotavirus antigen, negative; and E. coli O157 polymerase chain reaction, negative. Blood, urine, and stool cultures were negative. Posterior-anterior chest radiograph was normal. An abdominal ultrasonogram revealed mild thickening of the wall of the rectum and the sigmoid colon, but was otherwise normal. Follow-up laboratory findings were shown in Table 1. A diagnosis of sepsis and idiopathic thrombocytopenia was made and the patient was treated with antibiotics (ceftriaxone and metronidazole). Intravenous immunoglobulin (5.5 grams per day, total 11 g) was infused on the third and fourth hospital days. Packed RBCs (100 mL [10 mL/kg]) were transfused on the fourth hospital day because the hemoglobin fell to 7.7 g/L. From the third hospital day onward, the patient did not have any bloody stools. He gradually returned to normal as his diarrhea and oral intake improved. On the ninth hospital day, he was discharged. No further medication was prescribed. A 6-month follow-up was done. His vital signs were normal during this period. He did not develop any related symptoms. All laboratory findings were normal except for persistent microscopic hematuria.
Discussion
Initially, it was difficult to diagnose this case. The two possible diagnoses were Evans syndrome (ES) associated with glomerulonephritis, or APSGN associated with idiopathic thrombocytopenia.
ES is recognized as a special variant of autoimmune hemolytic anemia (AIHA). It is characterized by the presence of two or more hematologic immune cytopenias, most often AIHA and idiopathic thrombocytopenic purpura (ITP) [3]. ES may be a manifestation of systemic lupus erythematosus (SLE), common variable immune deficiency, autoimmune lymphoproliferative disorder, or any other immune disorder [4]. The direct Coombs test is positive in 95% cases of AIHA [5]. The main differential diagnoses of ES include leukemia, other lymphoproliferative disorders, SLE, scleroderma, mixed connective tissue disease, Hashimoto’s thyroiditis, hemolytic uremic syndrome (HUS), thrombotic thrombocytopenic purpura (TTP), liver cirrhosis, sarcoidosis, and amyloidosis [5]. SLE was excluded in this case because fluorescent antinuclear antibody and anti-double stranded-DNA antibody were negative. Typical TTP or HUS was excluded because no neurological symptoms or evidence of renal failure was present. The association of ES with glomerulonephritis has not been previously reported. Erythropoiesis induced by anemia should raise the reticulocyte count to 4-5% [6]. However, some patients with acute hemolysis do not show the expected degree of reticulocytosis. Most probably, this may be due to a lag in marrow responsiveness to hemolytic stress [6]. In this case, clinical evidence did not support the diagnosis of ES or any of its differentials, except hemolytic anemia and ITP.
APSGN, resulting from a prior infection with group A β-hemolytic streptococcus, is one of the most common renal diseases [7]. APSGN most commonly occurs in children 5 to 12 years old [7]. The most popular theory of the pathogenic mechanism of APSGN is the immune-complex theory; this involves glomerular deposition of nephritogenic streptococcal antigen and subsequent formation of immune complexes in situ, and/or deposition of circulating antigen-antibody complexes [8]. Two antigens have been actively investigated as potential causes of APSGN: the nephritis-associated plasmin receptor, also known as streptococcal glyceraldehyde-3-phosphate dehydrogenase, and the cationic cysteine proteinase known as streptococcal pyogenic exotoxin B [9].
Patients with APSGN sometimes exhibit atypical or unusual clinical manifestations, which may result in delayed diagnosis [10]. Atypical manifestations of APSGN can be classified as follows: co-occurrence of immune-mediated diseases; non-immune-mediated complications; and unusual clinical presentations or courses [11]. Immune-mediated diseases include acute rheumatic fever, poststreptococcal reactive arthritis, vasculitis, immune thrombocytopenic purpura, AIHA, diffuse alveolar hemorrhage, and uveitis [11]. Non-immune-mediated complications include posterior reversible encephalopathy syndrome, thrombotic microangiopathy, and gallbladder wall thickening [11]. Unusual clinical presentations or courses include minimal urinary abnormalities and recurrence [11]. AIHA is a clinical condition in which IgG and/or IgM antibodies bind to RBC surface antigens and initiate RBC destruction via the complement and reticuloendothelial systems [12]. Some case reports of the development of ITP in APSGN followed the first report by Kaplan and Esseltine [13, 14]. All patients described in these case reports improved after treatment with corticosteroid or immunoglobulin therapy. Although the precise pathogenic mechanism for the development of ITP in patients with APSGN is unclear, Muguruma et al. speculated about the pathogenesis of associated diseases through production of autoantibodies cross-reactive against group A streptococcus and platelets [14]. In our case, Coombs negative AIHA and ITP might have been considered atypical presentations of APSGN. However, ASO titer on admission was negative and renal biopsy was not performed, because of the following reasons: there were mild respiratory symptoms five days before the development of hematuria; serum C3 level was lower than normal during the acute stage, and then remarkably increased to the normal level after 3 weeks; proteinuria improved within a short time period during the disease course without specific treatment; APSGN is the most common glomerulonephritis related to a previous episode of infection; ASO can be negative in 10% of patients with APSGN [15]; clinical findings, except for microscopic hematuria, resolved completely with Ig infusion and RBC transfusion; mild forms of renal microangiophy, like TTP or HUS, cannot be completely excluded in this case, because they can initially present with only microangiopathic hemolytic anemia and thrombocytopenia, without renal failure [16], and because low C3 level can be detected in 50% of patients with HUS [17]. However, many patients with TTP or HUS progress to acute renal failure if plasmapheresis is not performed early, and low C3 levels in HUS usually do not recover to normal within a short time period during the disease course.
Postinfectious glomerulonephritis (PIGN) would be more appropriate than APSGN as the diagnosis. However, we did not find reports of PIGN coexistent with hemolytic anemia (HA) and thrombocytopenia in the literature. There were only two adult cases with PIGN coexistent with TTP, who progressed to acute renal failure.
We thought the diarrhea originated from coinfection of the gastrointestinal tract through prior infection with other organisms, and was not related to the development of the hematological findings or renal symptoms. We did not find reports of gastrointestinal diseases coexistent with low C3 or nephritic symptoms without other associated diseases in the literature.
We thought his hypokalemia might be caused by gastrointestinal loss and poor oral intake, because the urine potassium was less than 15 mmol/L, and the transtubular potassium gradient was less than 4 on admission.
In conclusion, patients with APSGN sometimes exhibit atypical or unusual clinical manifestations, which may result in delayed diagnosis or misdiagnosis. Timely recognition of these manifestations is important in order to ensure adequate treatment in such patients.
Notes
Conflict of Interest
The authors declare that they have no conflict of interest.
Financial Disclosure
The authors declare that no financial or material support was received for this research.